Patient Questionnaire
ADVERTISEMENT
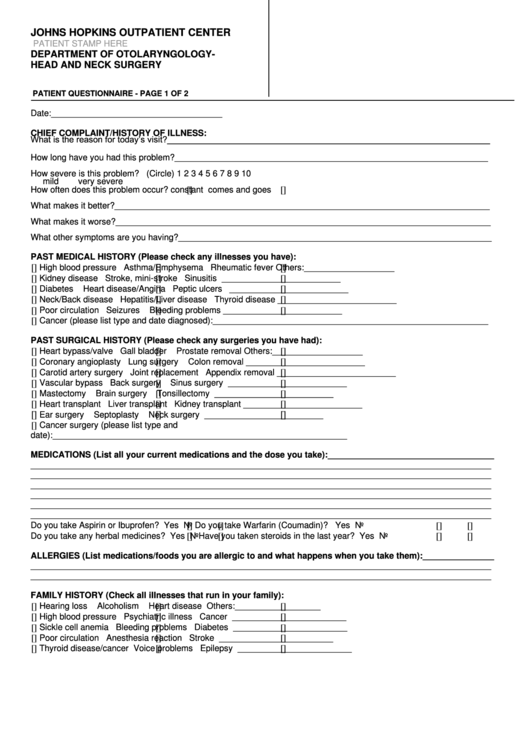
JOHNS HOPKINS OUTPATIENT CENTER
PATIENT STAMP HERE
DEPARTMENT OF OTOLARYNGOLOGY-
HEAD AND NECK SURGERY
PATIENT QUESTIONNAIRE - PAGE 1 OF 2
Date:____________________________________
CHIEF COMPLAINT/HISTORY OF ILLNESS:
What is the reason for today’s visit?____________________________________________________________________
How long have you had this problem?__________________________________________________________________
How severe is this problem? (Circle)
1
2
3
4
5
6
7
8
9
10
mild
very severe
How often does this problem occur?
constant
comes and goes
What makes it better?_______________________________________________________________________________
What makes it worse?_______________________________________________________________________________
What other symptoms are you having?__________________________________________________________________
PAST MEDICAL HISTORY (Please check any illnesses you have):
High blood pressure
Asthma/Emphysema
Rheumatic fever
Others:___________________
Kidney disease
Stroke, mini-stroke
Sinusitis
_________________________
Diabetes
Heart disease/Angina
Peptic ulcers
_________________________
Neck/Back disease
Hepatitis/Liver disease
Thyroid disease
_________________________
Poor circulation
Seizures
Bleeding problems
_________________________
Cancer (please list type and date diagnosed):__________________________________________________________
PAST SURGICAL HISTORY (Please check any surgeries you have had):
Heart bypass/valve
Gall bladder
Prostate removal
Others:___________________
Coronary angioplasty
Lung surgery
Colon removal
_________________________
Carotid artery surgery
Joint replacement
Appendix removal
_________________________
Vascular bypass
Back surgery
Sinus surgery
_________________________
Mastectomy
Brain surgery
Tonsillectomy
_________________________
Heart transplant
Liver transplant
Kidney transplant
_________________________
Ear surgery
Septoplasty
Neck surgery
_________________________
Cancer surgery (please list type and
date):______________________________________________________________
MEDICATIONS (List all your current medications and the dose you take):___________________________________
_________________________________________________________________________________________________
_________________________________________________________________________________________________
_________________________________________________________________________________________________
_________________________________________________________________________________________________
_________________________________________________________________________________________________
_________________________________________________________________________________________________
Do you take Aspirin or Ibuprofen?
Yes
No
Do you take Warfarin (Coumadin)?
Yes
No
Do you take any herbal medicines?
Yes
No
Have you taken steroids in the last year?
Yes
No
ALLERGIES (List medications/foods you are allergic to and what happens when you take them):_______________
_________________________________________________________________________________________________
_________________________________________________________________________________________________
FAMILY HISTORY (Check all illnesses that run in your family):
Hearing loss
Alcoholism
Heart disease
Others:__________________
High blood pressure
Psychiatric illness
Cancer
________________________
Sickle cell anemia
Bleeding problems
Diabetes
________________________
Poor circulation
Anesthesia reaction
Stroke
________________________
Thyroid disease/cancer
Voice problems
Epilepsy
________________________
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2 3
3








