Sample Care Plan Template
ADVERTISEMENT
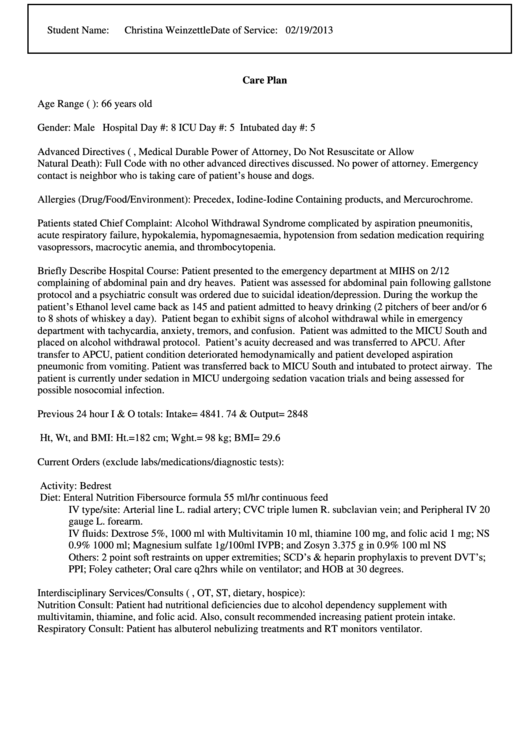
Student Name:
Christina Weinzettle
Date of Service: 02/19/2013
Care Plan
Age Range (e.g. 60-65 yr): 66 years old
Gender: Male
Hospital Day #: 8
ICU Day #: 5
Intubated day #: 5
Advanced Directives (e.g. Living Will, Medical Durable Power of Attorney, Do Not Resuscitate or Allow
Natural Death): Full Code with no other advanced directives discussed. No power of attorney. Emergency
contact is neighbor who is taking care of patient’s house and dogs.
Allergies (Drug/Food/Environment): Precedex, Iodine-Iodine Containing products, and Mercurochrome.
Patients stated Chief Complaint: Alcohol Withdrawal Syndrome complicated by aspiration pneumonitis,
acute respiratory failure, hypokalemia, hypomagnesaemia, hypotension from sedation medication requiring
vasopressors, macrocytic anemia, and thrombocytopenia.
Briefly Describe Hospital Course: Patient presented to the emergency department at MIHS on 2/12
complaining of abdominal pain and dry heaves. Patient was assessed for abdominal pain following gallstone
protocol and a psychiatric consult was ordered due to suicidal ideation/depression. During the workup the
patient’s Ethanol level came back as 145 and patient admitted to heavy drinking (2 pitchers of beer and/or 6
to 8 shots of whiskey a day). Patient began to exhibit signs of alcohol withdrawal while in emergency
department with tachycardia, anxiety, tremors, and confusion. Patient was admitted to the MICU South and
placed on alcohol withdrawal protocol. Patient’s acuity decreased and was transferred to APCU. After
transfer to APCU, patient condition deteriorated hemodynamically and patient developed aspiration
pneumonic from vomiting. Patient was transferred back to MICU South and intubated to protect airway. The
patient is currently under sedation in MICU undergoing sedation vacation trials and being assessed for
possible nosocomial infection.
Previous 24 hour I & O totals: Intake= 4841. 74 & Output= 2848
Ht, Wt, and BMI: Ht.=182 cm; Wght.= 98 kg; BMI= 29.6
Current Orders (exclude labs/medications/diagnostic tests):
Activity: Bedrest
Diet: Enteral Nutrition Fibersource formula 55 ml/hr continuous feed
IV type/site: Arterial line L. radial artery; CVC triple lumen R. subclavian vein; and Peripheral IV 20
gauge L. forearm.
IV fluids: Dextrose 5%, 1000 ml with Multivitamin 10 ml, thiamine 100 mg, and folic acid 1 mg; NS
0.9% 1000 ml; Magnesium sulfate 1g/100ml IVPB; and Zosyn 3.375 g in 0.9% 100 ml NS
Others: 2 point soft restraints on upper extremities; SCD’s & heparin prophylaxis to prevent DVT’s;
PPI; Foley catheter; Oral care q2hrs while on ventilator; and HOB at 30 degrees.
Interdisciplinary Services/Consults (e.g. PT, OT, ST, dietary, hospice):
Nutrition Consult: Patient had nutritional deficiencies due to alcohol dependency supplement with
multivitamin, thiamine, and folic acid. Also, consult recommended increasing patient protein intake.
Respiratory Consult: Patient has albuterol nebulizing treatments and RT monitors ventilator.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2 3
3 4
4 5
5 6
6 7
7 8
8 9
9 10
10 11
11 12
12 13
13 14
14 15
15 16
16 17
17 18
18 19
19 20
20 21
21 22
22 23
23 24
24 25
25 26
26 27
27 28
28 29
29 30
30 31
31 32
32 33
33 34
34 35
35 36
36 37
37 38
38 39
39 40
40 41
41 42
42 43
43 44
44 45
45 46
46 47
47 48
48 49
49 50
50 51
51








