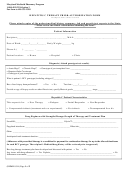
Michigan Prior Authorization Request Form
For Prescription Drugs
Instructions
Important: Please read all instructions below before completing FIS 2288.
Section 2212c of Public Act 218 of 1956, MCL 500.2212c, requires the use of a standard prior authorization form
when a policy, certificate or contract requires prior authorization for prescription drug benefits.
A standard form, FIS 2288, is being made available by the Department of Insurance and Financial Services to
simplify exchanges of information between prescribers and health insurers as part of the process of requesting
prescription drug prior authorization. This form will be updated periodically and the form number and most
recent revision date are displayed in the top left-hand corner.
This form is made available for use by prescribers to initiate a prior authorization request with the
health insurer.
Prior authorization requests are defined as requests for pre-approval from an insurer for specified
medications before they are dispensed.
“Prescriber” means the term as defined in section 17708 of the Public Health Code, 1978 PA 368, MCL
333.17708.
“Prescription drug” means the term as defined in section 17708 of the Public Health Code, 1978 PA 368,
MCL 333.17708.
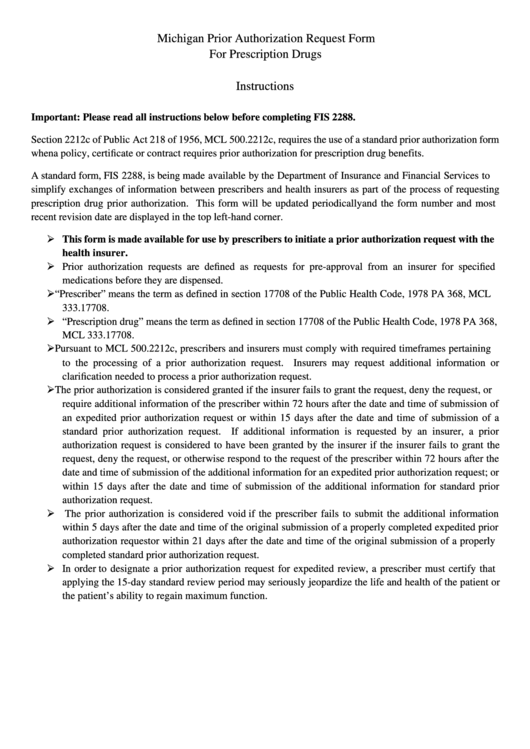
Pursuant to MCL 500.2212c, prescribers and insurers must comply with required timeframes pertaining
to the processing of a prior authorization request. Insurers may request additional information or
clarification needed to process a prior authorization request.
The prior authorization is considered granted if the insurer fails to grant the request, deny the request, or
require additional information of the prescriber within 72 hours after the date and time of submission of
an expedited prior authorization request or within 15 days after the date and time of submission of a
standard prior authorization request. If additional information is requested by an insurer, a prior
authorization request is considered to have been granted by the insurer if the insurer fails to grant the
request, deny the request, or otherwise respond to the request of the prescriber within 72 hours after the
date and time of submission of the additional information for an expedited prior authorization request; or
within 15 days after the date and time of submission of the additional information for standard prior
authorization request.
The prior authorization is considered void if the prescriber fails to submit the additional information
within 5 days after the date and time of the original submission of a properly completed expedited prior
authorization request or within 21 days after the date and time of the original submission of a properly
completed standard prior authorization request.
In order to designate a prior authorization request for expedited review, a prescriber must certify that
applying the 15-day standard review period may seriously jeopardize the life and health of the patient or
the patient’s ability to regain maximum function.
 1
1 2
2 3
3