Request Form For Prior Authorization Nonsteroidal Anti-Inflammatory Drugs - Iowa Department Of Human Services
ADVERTISEMENT
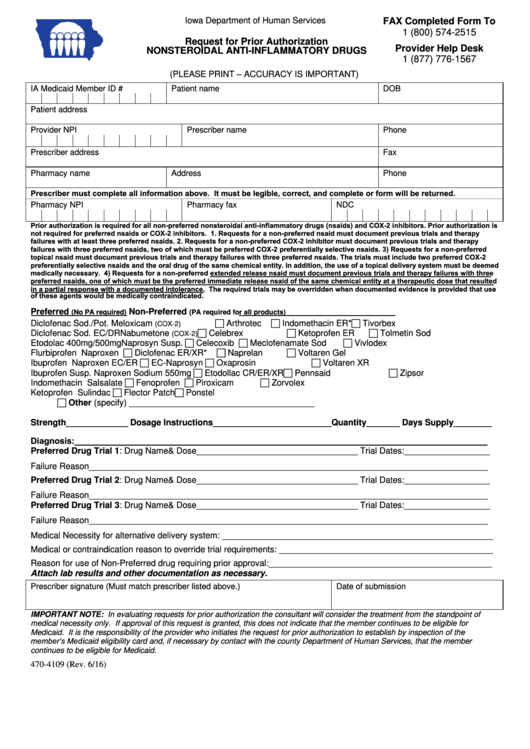
Iowa Department of Human Services
FAX Completed Form To
1 (800) 574-2515
Request for Prior Authorization
Provider Help Desk
NONSTEROIDAL ANTI-INFLAMMATORY DRUGS
1 (877) 776-1567
(PLEASE PRINT – ACCURACY IS IMPORTANT)
IA Medicaid Member ID #
Patient name
DOB
Patient address
Provider NPI
Prescriber name
Phone
Prescriber address
Fax
Pharmacy name
Address
Phone
Prescriber must complete all information above. It must be legible, correct, and complete or form will be returned.
Pharmacy NPI
Pharmacy fax
NDC
Prior authorization is required for all non-preferred nonsteroidal anti-inflammatory drugs (nsaids) and COX-2 inhibitors. Prior authorization is
not required for preferred nsaids or COX-2 inhibitors. 1. Requests for a non-preferred nsaid must document previous trials and therapy
failures with at least three preferred nsaids. 2. Requests for a non-preferred COX-2 inhibitor must document previous trials and therapy
failures with three preferred nsaids, two of which must be preferred COX-2 preferentially selective nsaids. 3) Requests for a non-preferred
topical nsaid must document previous trials and therapy failures with three preferred nsaids. The trials must include two preferred COX-2
preferentially selective nsaids and the oral drug of the same chemical entity. In addition, the use of a topical delivery system must be deemed
medically necessary. 4) Requests for a non-preferred extended release nsaid must document previous trials and therapy failures with three
preferred nsaids, one of which must be the preferred immediate release nsaid of the same chemical entity at a therapeutic dose that resulted
in a partial response with a documented intolerance. The required trials may be overridden when documented evidence is provided that use
of these agents would be medically contraindicated.
Preferred
Non-Preferred
(No PA required)
(PA required for all products)
Arthrotec
Indomethacin ER*
Tivorbex
Diclofenac Sod./Pot.
Meloxicam
(COX-2)
Celebrex
Ketoprofen ER
Tolmetin Sod
Diclofenac Sod. EC/DR
Nabumetone
(COX-2)
Celecoxib
Meclofenamate Sod
Vivlodex
Etodolac 400mg/500mg
Naprosyn Susp.
Diclofenac ER/XR*
Naprelan
Voltaren Gel
Flurbiprofen
Naproxen
EC-Naprosyn
Oxaprosin
Voltaren XR
Ibuprofen
Naproxen EC/ER
Naproxen Sodium 550mg Etodollac CR/ER/XR Pennsaid
Zipsor
Ibuprofen Susp.
Fenoprofen
Piroxicam
Zorvolex
Indomethacin
Salsalate
Flector Patch
Ponstel
Ketoprofen
Sulindac
Other (specify) _______________________________________
Strength_____________ Dosage Instructions_________________________Quantity_______ Days Supply________
Diagnosis:_______________________________________________________________________________________
Preferred Drug Trial 1: Drug Name& Dose__________________________________ Trial Dates:__________________
Failure Reason____________________________________________________________________________________
Preferred Drug Trial 2: Drug Name& Dose__________________________________ Trial Dates:__________________
Failure Reason____________________________________________________________________________________
Preferred Drug Trial 3: Drug Name& Dose__________________________________ Trial Dates:__________________
Failure Reason____________________________________________________________________________________
Medical Necessity for alternative delivery system: _________________________________________________________
Medical or contraindication reason to override trial requirements: _____________________________________________
Reason for use of Non-Preferred drug requiring prior approval:_______________________________________________
Attach lab results and other documentation as necessary.
Prescriber signature (Must match prescriber listed above.)
Date of submission
IMPORTANT NOTE: In evaluating requests for prior authorization the consultant will consider the treatment from the standpoint of
medical necessity only. If approval of this request is granted, this does not indicate that the member continues to be eligible for
Medicaid. It is the responsibility of the provider who initiates the request for prior authorization to establish by inspection of the
member’s Medicaid eligibility card and, if necessary by contact with the county Department of Human Services, that the member
continues to be eligible for Medicaid.
470-4109 (Rev. 6/16)
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1








