Medical History Form
ADVERTISEMENT
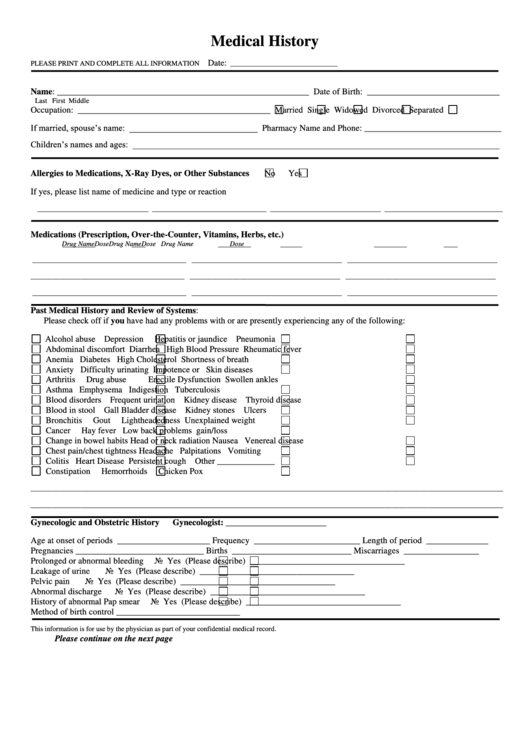
Medical History
Date:
PLEASE PRINT AND COMPLETE ALL INFORMATION
______________________________
Name: _________________________________________________________ Date of Birth: ______________________________
Last
First
Middle
Occupation: ____________________________________________
Married
Single
Widowed
Divorced
Separated
If married, spouse’s name: _____________________________ Pharmacy Name and Phone: _______________________________
Children’s names and ages: ___________________________________________________________________________________
Allergies to Medications, X-Ray Dyes, or Other Substances
No
Yes
If yes, please list name of medicine and type or reaction
_______________________________ ________________________________ _______________________________ _________________________________
Medications (Prescription, Over-the-Counter, Vitamins, Herbs, etc.)
Drug Name
Dose
Drug Name
Dose
Drug Name
Dose
___________________________________________ __________________________________________ __________________________________________
___________________________________________ __________________________________________ __________________________________________
___________________________________________ __________________________________________ __________________________________________
Past Medical History and Review of Systems:
Please check off if you have had any problems with or are presently experiencing any of the following:
Alcohol abuse
Depression
Hepatitis or jaundice
Pneumonia
Abdominal discomfort
Diarrhea
High Blood Pressure
Rheumatic fever
Anemia
Diabetes
High Cholesterol
Shortness of breath
Anxiety
Difficulty urinating
Impotence or
Skin diseases
Arthritis
Drug abuse
Erectile Dysfunction
Swollen ankles
Asthma
Emphysema
Indigestion
Tuberculosis
Blood disorders
Frequent urination
Kidney disease
Thyroid disease
Blood in stool
Gall Bladder disease
Kidney stones
Ulcers
Bronchitis
Gout
Lightheadedness
Unexplained weight
Cancer
Hay fever
Low back problems
gain/loss
Change in bowel habits
Head or neck radiation
Nausea
Venereal disease
Chest pain/chest tightness
Headache
Palpitations
Vomiting
Colitis
Heart Disease
Persistent cough
Other _____________
Constipation
Hemorrhoids
Chicken Pox
____________________________________________________________________________________________________________________________________
____________________________________________________________________________________________________________________________________
Gynecologic and Obstetric History
Gynecologist: _______________________
Age at onset of periods _____________________
Frequency ________________________
Length of period ______________
Pregnancies _____________________________
Births ___________________________
Miscarriages _________________
Prolonged or abnormal bleeding
No
Yes (Please describe) ___________________________________
Leakage of urine
No
Yes (Please describe) ___________________________________
Pelvic pain
No
Yes (Please describe) ___________________________________
Abnormal discharge
No
Yes (Please describe) ___________________________________
History of abnormal Pap smear
No
Yes (Please describe) ___________________________________
Method of birth control ____________________________
This information is for use by the physician as part of your confidential medical record.
Please continue on the next page
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2








