Appeal Request Form
Download a blank fillable Appeal Request Form in PDF format just by clicking the "DOWNLOAD PDF" button.
Open the file in any PDF-viewing software. Adobe Reader or any alternative for Windows or MacOS are required to access and complete fillable content.
Complete Appeal Request Form with your personal data - all interactive fields are highlighted in places where you should type, access drop-down lists or select multiple-choice options.
Some fillable PDF-files have the option of saving the completed form that contains your own data for later use or sending it out straight away.
ADVERTISEMENT
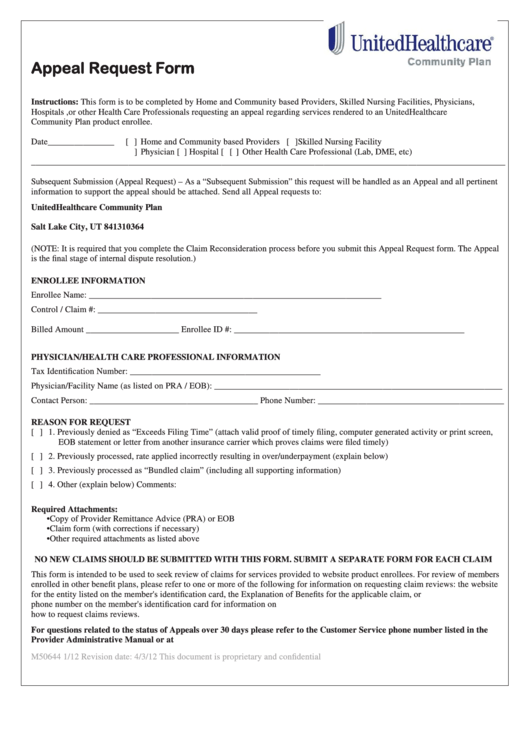
Appeal Request Form
Instructions: This form is to be completed by Home and Community based Providers, Skilled Nursing Facilities, Physicians,
Hospitals ,or other Health Care Professionals requesting an appeal regarding services rendered to an UnitedHealthcare
Community Plan product enrollee.
Date_______________
[ ] Home and Community based Providers [ ]Skilled Nursing Facility
[
] Physician [ ] Hospital [
] Other Health Care Professional (Lab, DME, etc)
___________________________________________________________________________________________________________
Subsequent Submission (Appeal Request) – As a “Subsequent Submission” this request will be handled as an Appeal and all pertinent
information to support the appeal should be attached. Send all Appeal requests to:
UnitedHealthcare Community Plan
P.O. Box 31364
Salt Lake City, UT 841310364
(NOTE: It is required that you complete the Claim Reconsideration process before you submit this Appeal Request form. The Appeal
is the final stage of internal dispute resolution.)
ENROLLEE INFORMATION
Enrollee Name: __________________________________________________________________D.O.B. ______________________
Control / Claim #: ____________________________________ D.O.S.___________________________
Billed Amount _____________________ Enrollee ID #: ____________________________________________________
PHYSICIAN/HEALTH CARE PROFESSIONAL INFORMATION
Tax Identification Number: ___________________________________________
Physician/Facility Name (as listed on PRA / EOB): _________________________________________________________________
Contact Person: ______________________________________ Phone Number: __________________________________________
REASON FOR REQUEST
[ ] 1. Previously denied as “Exceeds Filing Time” (attach valid proof of timely filing, computer generated activity or print screen,
EOB statement or letter from another insurance carrier which proves claims were filed timely)
[ ] 2. Previously processed, rate applied incorrectly resulting in over/underpayment (explain below)
[ ] 3. Previously processed as “Bundled claim” (including all supporting information)
[ ] 4. Other (explain below) Comments:
Required Attachments:
• Copy of Provider Remittance Advice (PRA) or EOB
• Claim form (with corrections if necessary)
• Other required attachments as listed above
NO NEW CLAIMS SHOULD BE SUBMITTED WITH THIS FORM. SUBMIT A SEPARATE FORM FOR EACH CLAIM
This form is intended to be used to seek review of claims for services provided to website product enrollees. For review of members
enrolled in other benefit plans, please refer to one or more of the following for information on requesting claim reviews: the website
for the entity listed on the member's identification card, the Explanation of Benefits for the applicable claim, or
You may also call the telephone number on the member's identification card for information on
how to request claims reviews.
For questions related to the status of Appeals over 30 days please refer to the Customer Service phone number listed in the
Provider Administrative Manual or at .
M50644 1/12 Revision date: 4/3/12
This document is proprietary and confidential
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1








