Prescription Claim Form
ADVERTISEMENT
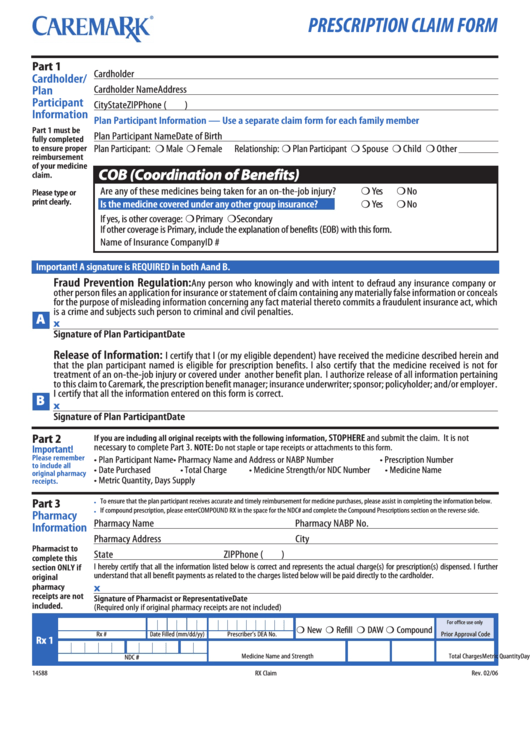
PRESCRIPTION CLAIM FORM
Part 1
Cardholder ID No.
Group No./Group Name
Cardholder/
Cardholder Name
Address
Plan
Participant
City
State
ZIP
Phone (
)
Information
Plan Participant Information — Use a separate claim form for each family member
Part 1 must be
Plan Participant Name
Date of Birth
Plan Participant: H Male H Female
Relationship: H Plan Participant H Spouse H Child H Other
fully completed
to ensure proper
reimbursement
of your medicine
COB (Coordination of Benefits)
claim.
H Yes
H No
Are any of these medicines being taken for an on-the-job injury?
Please type or
H Yes
H No
print clearly.
Is the medicine covered under any other group insurance?
If yes, is other coverage: H Primary H Secondary
If other coverage is Primary, include the explanation of benefits (EOB) with this form.
Name of Insurance Company
ID #
Important! A signature is REQUIRED in both A and B.
Fraud Prevention Regulation:
Any person who knowingly and with intent to defraud any insurance company or
other person files an application for insurance or statement of claim containing any materially false information or conceals
for the purpose of misleading information concerning any fact material thereto commits a fraudulent insurance act, which
is a crime and subjects such person to criminal and civil penalties.
A
x
Signature of Plan Participant
Date
Release of Information:
I certify that I (or my eligible dependent) have received the medicine described herein and
that the plan participant named is eligible for prescription benefits. I also certify that the medicine received is not for
treatment of an on-the-job injury or covered under another benefit plan. I authorize release of all information pertaining
to this claim to Caremark, the prescription benefit manager; insurance underwriter; sponsor; policyholder; and/or employer.
I certify that all the information entered on this form is correct.
B
x
Signature of Plan Participant
Date
STOP HERE and submit the claim. It is not
Part 2
If you are including all original receipts with the following information,
necessary to complete Part 3.
NOTE: Do not staple or tape receipts or attachments to this form.
Important!
Please remember
• Plan Participant Name • Pharmacy Name and Address or NABP Number
• Prescription Number
to include all
• Date Purchased
• Total Charge
• Medicine Strength/or NDC Number
• Medicine Name
original pharmacy
• Metric Quantity, Days Supply
receipts.
To ensure that the plan participant receives accurate and timely reimbursement for medicine purchases, please assist in completing the information below.
Part 3
•
If compound prescription, please enter COMPOUND RX in the space for the NDC # and complete the Compound Prescriptions section on the reverse side.
•
Pharmacy
Pharmacy Name
Pharmacy NABP No.
Information
Pharmacy Address
City
Pharmacist to
State
ZIP
Phone (
)
complete this
I hereby certify that all the information listed below is correct and represents the actual charge(s) for prescription(s) dispensed. I further
section ONLY if
understand that all benefit payments as related to the charges listed below will be paid directly to the cardholder.
original
pharmacy
x
receipts are not
Signature of Pharmacist or Representative
Date
included.
(Required only if original pharmacy receipts are not included)
H New H Refill H DAW H Compound
For office use only
Rx #
Date Filled (mm/dd/yy)
Prescriber’s DEA No.
Prior Approval Code
Rx 1
Medicine Name and Strength
Metric Quantity
Days Supply
Total Charges
NDC #
14588
Rev. 02/06
RX Claim
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1 2
2








