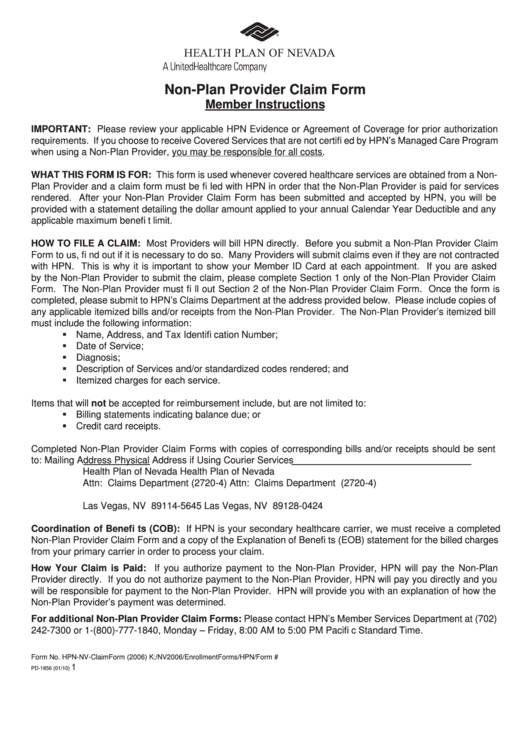
Non-Plan Provider Claim Form
ADVERTISEMENT
Non-Plan Provider Claim Form
Member Instructions
IMPORTANT: Please review your applicable HPN Evidence or Agreement of Coverage for prior authorization
requirements. If you choose to receive Covered Services that are not certifi ed by HPN’s Managed Care Program
when using a Non-Plan Provider, you may be responsible for all costs.
WHAT THIS FORM IS FOR: This form is used whenever covered healthcare services are obtained from a Non-
Plan Provider and a claim form must be fi led with HPN in order that the Non-Plan Provider is paid for services
rendered. After your Non-Plan Provider Claim Form has been submitted and accepted by HPN, you will be
provided with a statement detailing the dollar amount applied to your annual Calendar Year Deductible and any
applicable maximum benefi t limit.
HOW TO FILE A CLAIM: Most Providers will bill HPN directly. Before you submit a Non-Plan Provider Claim
Form to us, fi nd out if it is necessary to do so. Many Providers will submit claims even if they are not contracted
with HPN. This is why it is important to show your Member ID Card at each appointment. If you are asked
by the Non-Plan Provider to submit the claim, please complete Section 1 only of the Non-Plan Provider Claim
Form. The Non-Plan Provider must fi ll out Section 2 of the Non-Plan Provider Claim Form. Once the form is
completed, please submit to HPN’s Claims Department at the address provided below. Please include copies of
any applicable itemized bills and/or receipts from the Non-Plan Provider. The Non-Plan Provider’s itemized bill
must include the following information:
Name, Address, and Tax Identifi cation Number;
Date of Service;
Diagnosis;
Description of Services and/or standardized codes rendered; and
Itemized charges for each service.
Items that will not be accepted for reimbursement include, but are not limited to:
Billing statements indicating balance due; or
Credit card receipts.
Completed Non-Plan Provider Claim Forms with copies of corresponding bills and/or receipts should be sent
to:
Mailing Address
Physical Address if Using Courier Services
Health Plan of Nevada
Health Plan of Nevada
Attn: Claims Department (2720-4)
Attn: Claims Department (2720-4)
P.O. Box 15645
2720 N. Tenaya Way
Las Vegas, NV 89114-5645
Las Vegas, NV 89128-0424
Coordination of Benefi ts (COB): If HPN is your secondary healthcare carrier, we must receive a completed
Non-Plan Provider Claim Form and a copy of the Explanation of Benefi ts (EOB) statement for the billed charges
from your primary carrier in order to process your claim.
How Your Claim is Paid: If you authorize payment to the Non-Plan Provider, HPN will pay the Non-Plan
Provider directly. If you do not authorize payment to the Non-Plan Provider, HPN will pay you directly and you
will be responsible for payment to the Non-Plan Provider. HPN will provide you with an explanation of how the
Non-Plan Provider’s payment was determined.
For additional Non-Plan Provider Claim Forms: Please contact HPN’s Member Services Department at (702)
242-7300 or 1-(800)-777-1840, Monday – Friday, 8:00 AM to 5:00 PM Pacifi c Standard Time.
Form No. HPN-NV-ClaimForm (2006)
K:/NV2006/EnrollmentForms/HPN/Form #
1
PD-1856 (01/10)
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1 2
2 3
3 4
4