Sbar - Nursing Communication Documentation Form
ADVERTISEMENT
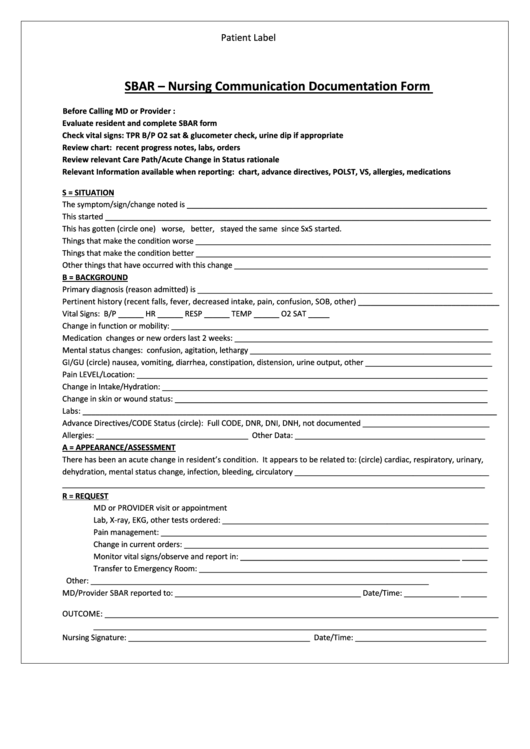
Patient Label
SBAR – Nursing Communication Documentation Form
Before Calling MD or Provider :
Evaluate resident and complete SBAR form
Check vital signs: TPR B/P O2 sat & glucometer check, urine dip if appropriate
Review chart: recent progress notes, labs, orders
Review relevant Care Path/Acute Change in Status rationale
Relevant Information available when reporting: chart, advance directives, POLST, VS, allergies, medications
S = SITUATION
The symptom/sign/change noted is _______________________________________________________________________
This started __________________________________________________________________________________________
This has gotten (circle one) worse, better, stayed the same since SxS started.
Things that make the condition worse _____________________________________________________________________
Things that make the condition better _____________________________________________________________________
Other things that have occurred with this change ____________________________________________________________
B = BACKGROUND
Primary diagnosis (reason admitted) is _____________________________________________________________________
Pertinent history (recent falls, fever, decreased intake, pain, confusion, SOB, other) _________________________________
Vital Signs: B/P ______ HR ______ RESP ______ TEMP ______ O2 SAT _____
Change in function or mobility: ___________________________________________________________________________
Medication changes or new orders last 2 weeks: _____________________________________________________________
Mental status changes: confusion, agitation, lethargy _________________________________________________________
GI/GU (circle) nausea, vomiting, diarrhea, constipation, distension, urine output, other ______________________________
Pain LEVEL/Location: ___________________________________________________________________________________
Change in Intake/Hydration: _____________________________________________________________________________
Change in skin or wound status: __________________________________________________________________________
Labs: ________________________________________________________________________________________________
Advance Directives/CODE Status (circle): Full CODE, DNR, DNI, DNH, not documented ______________________________
Allergies: ____________________________________ Other Data: _____________________________________________
A = APPEARANCE/ASSESSMENT
There has been an acute change in resident’s condition. It appears to be related to: (circle) cardiac, respiratory, urinary,
dehydration, mental status change, infection, bleeding, circulatory ______________________________________________
____________________________________________________________________________________________________
R = REQUEST
MD or PROVIDER visit or appointment
Lab, X-ray, EKG, other tests ordered: _______________________________________________________________
Pain management: _____________________________________________________________________________
Change in current orders: ________________________________________________________________________
Monitor vital signs/observe and report in: ____________________________________________________ ______
Transfer to Emergency Room: ____________________________________________________________________
Other: ________________________________________________________________________________
MD/Provider SBAR reported to: ____________________________________________ Date/Time: _____________ ______
OUTCOME: ___________________________________________________________________________________________
_____________________________________________________________________________________________
Nursing Signature: ___________________________________________ Date/Time: _______________________________
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1