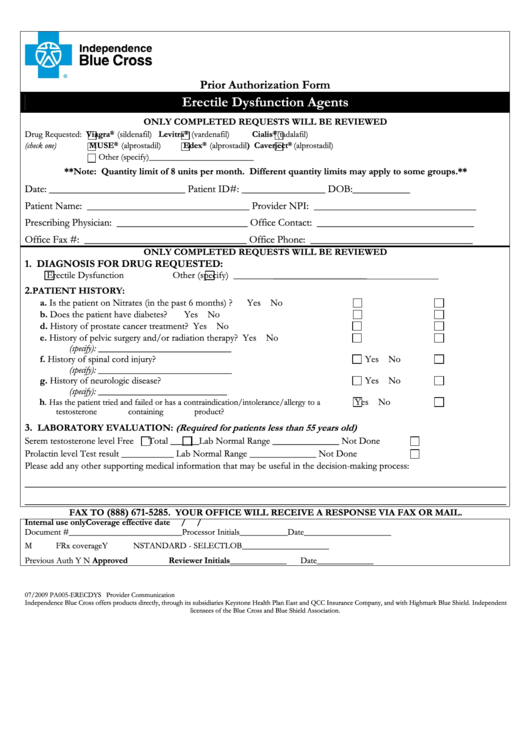
Prior Authorization Form - Erectile Dysfunction Agents
ADVERTISEMENT
Prior Authorization Form
Erectile Dysfunction Agents
ONLY COMPLETED REQUESTS WILL BE REVIEWED
Drug Requested:
Viagra
(sildenafil)
Levitra
(vardenafil)
Cialis
(tadalafil)
®
®
®
(check one)
MUSE
®
(alprostadil)
Edex
®
(alprostadil)
Caverject
®
(alprostadil)
Other (specify)________________________
**Note: Quantity limit of 8 units per month. Different quantity limits may apply to some groups.**
Date: __________________________
Patient ID#: ________________ DOB:___________
Patient Name: _______________________________
Provider NPI: _______________________________
Prescribing Physician: _________________________
Office Contact: ______________________________
Office Fax #: _______________________________
Office Phone: _______________________________
ONLY COMPLETED REQUESTS WILL BE REVIEWED
1. DIAGNOSIS FOR DRUG REQUESTED:
Erectile Dysfunction
Other (specify)
____________________________
2.
PATIENT HISTORY:
a. Is the patient on Nitrates (in the past 6 months) ?
Yes
No
b. Does the patient have diabetes?
Yes
No
d. History of prostate cancer treatment?
Yes
No
e. History of pelvic surgery and/or radiation therapy?
Yes
No
(specify): ____________________________
f. History of spinal cord injury?
Yes
No
(specify): ____________________________
g. History of neurologic disease?
Yes
No
(specify): ___________________________
h.
Yes
No
Has the patient tried and failed or has a contraindication/intolerance/allergy to a
testosterone containing product?
3.
LABORATORY EVALUATION:
(Required for patients less than 55 years old)
Serem testosterone level
Free
Total ______
Lab Normal Range ______________
Not Done
Prolactin level
Test result ___________
Lab Normal Range ______________
Not Done
Please add any other supporting medical information that may be useful in the decision-making process:
____________________________________________________________________________________________
____________________________________________________________________________________________
(888) 671-5285
FAX TO
. YOUR OFFICE WILL RECEIVE A RESPONSE VIA FAX OR MAIL.
Internal use only
Coverage effective date
/
/
Document #__________________________
Processor Initials___________
Date____________________
M
F
Rx coverage
Y
N
STANDARD - SELECT
LOB____________________
Previous Auth
Y
N
Approved
Reviewer Initials_____________
Date_____________
07/2009 PA005-ERECDYS
Provider Communication
Independence Blue Cross offers products directly, through its subsidiaries Keystone Health Plan East and QCC Insurance Company, and with Highmark Blue Shield. Independent
licensees of the Blue Cross and Blue Shield Association.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1