Medical History Form
ADVERTISEMENT
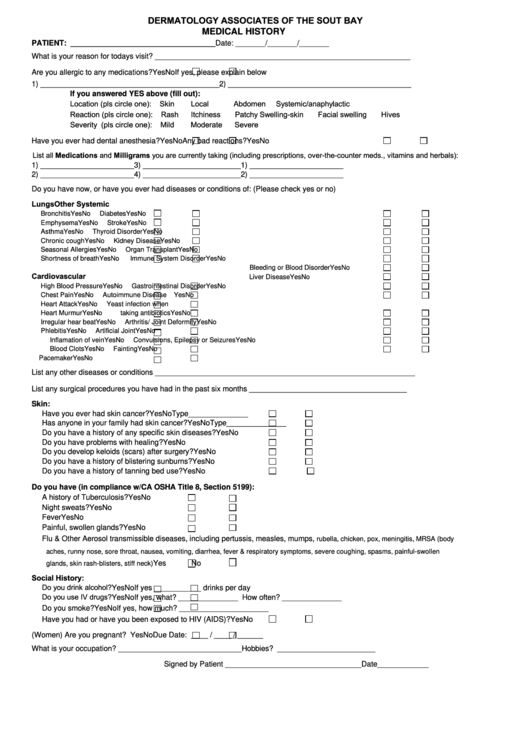
DERMATOLOGY ASSOCIATES OF THE SOUT BAY
MEDICAL HISTORY
PATIENT: __________________________________
Date: _______/_______/_______
What is your reason for todays visit? ____________________________________________________________
Are you allergic to any medications?
Yes
No
If yes, please explain below
1) __________________________________________
2) ___________________________________________
If you answered YES above (fill out):
Location (pls circle one):
Skin
Local
Abdomen Systemic/anaphylactic
Reaction (pls circle one):
Rash Itchiness Patchy Swelling-skin Facial swelling Hives
Severity (pls circle one):
Mild Moderate Severe
Have you ever had dental anesthesia?
Yes
No
Any bad reactions?
Yes
No
List all Medications and Milligrams you are currently taking (including prescriptions, over-the-counter meds., vitamins and herbals):
1) ______________________
3) _______________________
1) ______________________
2) ______________________
4) _______________________
2) ______________________
Do you have now, or have you ever had diseases or conditions of: (Please check yes or no)
Lungs
Other Systemic
Bronchitis
Yes
No
Diabetes
Yes
No
Emphysema
Yes
No
Stroke
Yes
No
Asthma
Yes
No
Thyroid Disorder
Yes
No
Chronic cough
Yes
No
Kidney Disease
Yes
No
Seasonal Allergies
Yes
No
Organ Transplant
Yes
No
Shortness of breath
Yes
No
Immune System Disorder
Yes
No
Bleeding or Blood Disorder
Yes
No
Cardiovascular
Liver Disease
Yes
No
High Blood Pressure
Yes
No
Gastrointestinal Disorder
Yes
No
Chest Pain
Yes
No
Autoimmune Disease
Yes
No
Heart Attack
Yes
No
Yeast infection when
Heart Murmur
Yes
No
taking antibiotics
Yes
No
Irregular hear beat
Yes
No
Arthritis/ Joint Deformity
Yes
No
Phlebitis
Yes
No
Artificial Joint
Yes
No
Inflamation of vein
Yes
No
Convulsions, Epilepsy or Seizures
Yes
No
Blood Clots
Yes
No
Fainting
Yes
No
Pacemaker
Yes
No
List any other diseases or conditions _____________________________________________________________
List any surgical procedures you have had in the past six months _____________________________________
Skin:
Have you ever had skin cancer?
Yes
No
Type______________
Has anyone in your family had skin cancer?
Yes
No
Type______________
Do you have a history of any specific skin diseases?
Yes
No
Do you have problems with healing?
Yes
No
Do you develop keloids (scars) after surgery?
Yes
No
Do you have a history of blistering sunburns?
Yes
No
Do you have a history of tanning bed use?
Yes
No
Do you have (in compliance w/CA OSHA Title 8, Section 5199):
A history of Tuberculosis?
Yes
No
Night sweats?
Yes
No
Fever
Yes
No
Painful, swollen glands?
Yes
No
Flu & Other Aerosol transmissible diseases, including pertussis, measles, mumps,
rubella, chicken, pox, meningitis, MRSA (body
aches, runny nose, sore throat, nausea, vomiting, diarrhea, fever & respiratory symptoms, severe coughing, spasms, painful-swollen
Yes
No
glands, skin rash-blisters, stiff neck)
Social History:
Do you drink alcohol?
Yes
No
If yes ___________ drinks per day
Do you use IV drugs?
Yes
No
If yes, what? ______________ How often? ______________
Do you smoke?
Yes
No
If yes, how much? _____________________
Have you had or have you been exposed to HIV (AIDS)?
Yes
No
(Women) Are you pregnant?
Yes
No
Due Date: ____ / ____ / ______
What is your occupation? _____________________________
Hobbies? _______________________
Signed by Patient ________________________________
Date____________
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1








