Enteral Nutrition - State Of New York Prior Authorization Of Benefits (Pab) Form
ADVERTISEMENT
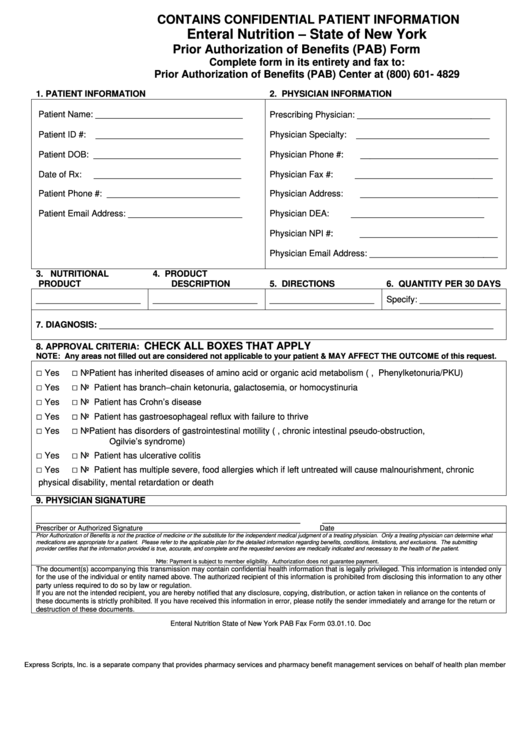
CONTAINS CONFIDENTIAL PATIENT INFORMATION
Enteral Nutrition – State of New York
Prior Authorization of Benefits (PAB) Form
Complete form in its entirety and fax to:
Prior Authorization of Benefits (PAB) Center at (800) 601- 4829
1. PATIENT INFORMATION
2. PHYSICIAN INFORMATION
Patient Name: _______________________________
Prescribing Physician: ____________________________
Patient ID #:
_______________________________
Physician Specialty:
____________________________
Patient DOB: _______________________________
Physician Phone #:
_____________________________
Date of Rx:
_______________________________
Physician Fax #:
_____________________________
Patient Phone #: ____________________________
Physician Address:
_____________________________
Patient Email Address: ________________________
Physician DEA:
____________________________
Physician NPI #:
_____________________________
Physician Email Address: ___________________________
3.
NUTRITIONAL
4.
PRODUCT
PRODUCT
DESCRIPTION
5. DIRECTIONS
6. QUANTITY PER 30 DAYS
______________________
______________________
______________________
Specify: _________________
7. DIAGNOSIS: ___________________________________________________________________________________
CHECK ALL BOXES THAT APPLY
8. APPROVAL CRITERIA:
NOTE: Any areas not filled out are considered not applicable to your patient & MAY AFFECT THE OUTCOME of this request.
□
□
Yes
No
Patient has inherited diseases of amino acid or organic acid metabolism (e.g., Phenylketonuria/PKU)
□
□
Yes
No
Patient has branch–chain ketonuria, galactosemia, or homocystinuria
□
□
Patient has Crohn’s disease
Yes
No
□
□
Yes
No
Patient has gastroesophageal reflux with failure to thrive
□
□
Yes
No
Patient has disorders of gastrointestinal motility (e.g., chronic intestinal pseudo-obstruction,
Ogilvie’s syndrome)
□
□
Yes
No
Patient has ulcerative colitis
□
□
Yes
No
Patient has multiple severe, food allergies which if left untreated will cause malnourishment, chronic
physical disability, mental retardation or death
9. PHYSICIAN SIGNATURE
____________________________________________________________
__________________________________________
Prescriber or Authorized Signature
Date
Prior Authorization of Benefits is not the practice of medicine or the substitute for the independent medical judgment of a treating physician. Only a treating physician can determine what
medications are appropriate for a patient. Please refer to the applicable plan for the detailed information regarding benefits, conditions, limitations, and exclusions. The submitting
provider certifies that the information provided is true, accurate, and complete and the requested services are medically indicated and necessary to the health of the patient.
Note: Payment is subject to member eligibility. Authorization does not guarantee payment.
The document(s) accompanying this transmission may contain confidential health information that is legally privileged. This information is intended only
for the use of the individual or entity named above. The authorized recipient of this information is prohibited from disclosing this information to any other
party unless required to do so by law or regulation.
If you are not the intended recipient, you are hereby notified that any disclosure, copying, distribution, or action taken in reliance on the contents of
these documents is strictly prohibited. If you have received this information in error, please notify the sender immediately and arrange for the return or
destruction of these documents.
Enteral Nutrition State of New York PAB Fax Form 03.01.10. Doc
Express Scripts, Inc. is a separate company that provides pharmacy services and pharmacy benefit management services on behalf of health plan members.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1








