Kalydeco (Ivacaftor) Prior Authorization Of Benefits (Pab) Form
ADVERTISEMENT
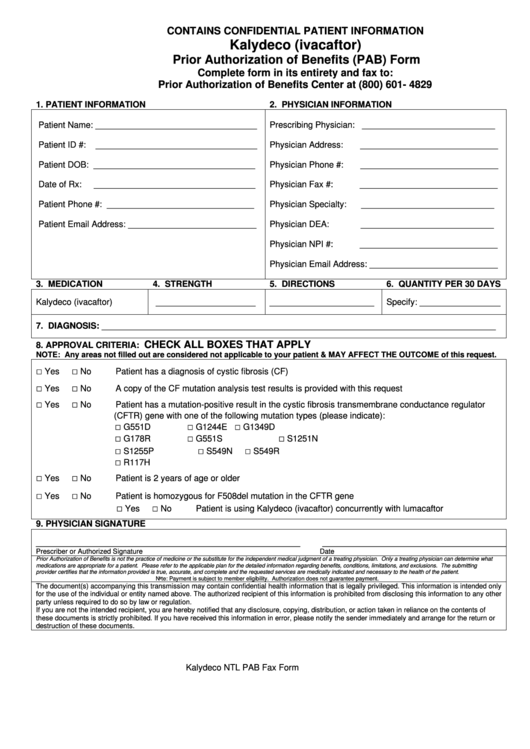
CONTAINS CONFIDENTIAL PATIENT INFORMATION
Kalydeco (ivacaftor)
Prior Authorization of Benefits (PAB) Form
Complete form in its entirety and fax to:
Prior Authorization of Benefits Center at (800) 601- 4829
1. PATIENT INFORMATION
2. PHYSICIAN INFORMATION
Patient Name: __________________________________
Prescribing Physician: ____________________________
Patient ID #:
__________________________________
Physician Address:
_____________________________
Patient DOB: __________________________________
Physician Phone #:
_____________________________
Date of Rx:
__________________________________
Physician Fax #:
_____________________________
Patient Phone #: _______________________________
Physician Specialty:
____________________________
Patient Email Address: ___________________________
Physician DEA:
____________________________
Physician NPI #:
_____________________________
Physician Email Address: ___________________________
3. MEDICATION
4. STRENGTH
5. DIRECTIONS
6. QUANTITY PER 30 DAYS
Kalydeco (ivacaftor)
_____________________
______________________
Specify: _________________
7. DIAGNOSIS: ___________________________________________________________________________________
CHECK ALL BOXES THAT APPLY
8. APPROVAL CRITERIA:
NOTE: Any areas not filled out are considered not applicable to your patient & MAY AFFECT THE OUTCOME of this request.
□
□
Yes
No
Patient has a diagnosis of cystic fibrosis (CF)
□
□
Yes
No
A copy of the CF mutation analysis test results is provided with this request
□
□
Yes
No
Patient has a mutation-positive result in the cystic fibrosis transmembrane conductance regulator
(CFTR) gene with one of the following mutation types (please indicate):
□
□
□
G551D
G1244E
G1349D
□
□
□
G178R
G551S
S1251N
□
□
□
S1255P
S549N
S549R
□
R117H
□
□
Yes
No
Patient is 2 years of age or older
□
□
Yes
No
Patient is homozygous for F508del mutation in the CFTR gene
□
□
Yes
No
Patient is using Kalydeco (ivacaftor) concurrently with lumacaftor
9. PHYSICIAN SIGNATURE
____________________________________________________________
__________________________________________
Prescriber or Authorized Signature
Date
Prior Authorization of Benefits is not the practice of medicine or the substitute for the independent medical judgment of a treating physician. Only a treating physician can determine what
medications are appropriate for a patient. Please refer to the applicable plan for the detailed information regarding benefits, conditions, limitations, and exclusions. The submitting
provider certifies that the information provided is true, accurate, and complete and the requested services are medically indicated and necessary to the health of the patient.
Note: Payment is subject to member eligibility. Authorization does not guarantee payment.
The document(s) accompanying this transmission may contain confidential health information that is legally privileged. This information is intended only
for the use of the individual or entity named above. The authorized recipient of this information is prohibited from disclosing this information to any other
party unless required to do so by law or regulation.
If you are not the intended recipient, you are hereby notified that any disclosure, copying, distribution, or action taken in reliance on the contents of
these documents is strictly prohibited. If you have received this information in error, please notify the sender immediately and arrange for the return or
destruction of these documents.
Kalydeco NTL PAB Fax Form 11.30.15.doc
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1








