Chart Review Audit Tool Form-Hospitals
ADVERTISEMENT
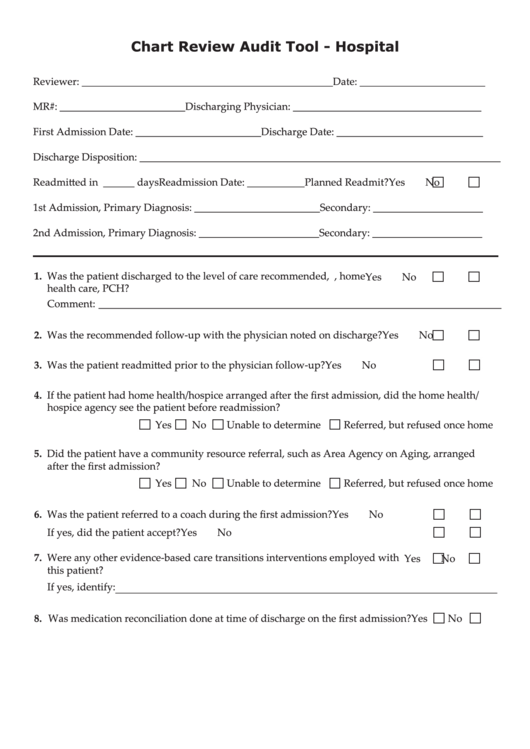
Chart Review Audit Tool - Hospital
Reviewer: ________________________________________________
Date: ________________________
MR#: ________________________
Discharging Physician: ____________________________________
First Admission Date: ________________________
Discharge Date: ____________________________
Discharge Disposition: _____________________________________________________________________
Readmitted in ______ days
Readmission Date: ___________
Planned Readmit?
Yes
No
1st Admission, Primary Diagnosis: ________________________
Secondary: _____________________
2nd Admission, Primary Diagnosis: _______________________
Secondary: _____________________
1. Was the patient discharged to the level of care recommended, e.g. SNF, home
Yes
No
health care, PCH?
Comment: _____________________________________________________________________________
2. Was the recommended follow-up with the physician noted on discharge?
Yes
No
3. Was the patient readmitted prior to the physician follow-up?
Yes
No
4. If the patient had home health/hospice arranged after the first admission, did the home health/
hospice agency see the patient before readmission?
Yes
No
Unable to determine
Referred, but refused once home
5. Did the patient have a community resource referral, such as Area Agency on Aging, arranged
after the first admission?
Yes
No
Unable to determine
Referred, but refused once home
6. Was the patient referred to a coach during the first admission?
Yes
No
If yes, did the patient accept?
Yes
No
7. Were any other evidence-based care transitions interventions employed with
Yes
No
this patient?
If yes, identify: _________________________________________________________________________
8. Was medication reconciliation done at time of discharge on the first admission?
Yes
No
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2








