Well Child Visit Form - 7-9 Months
ADVERTISEMENT
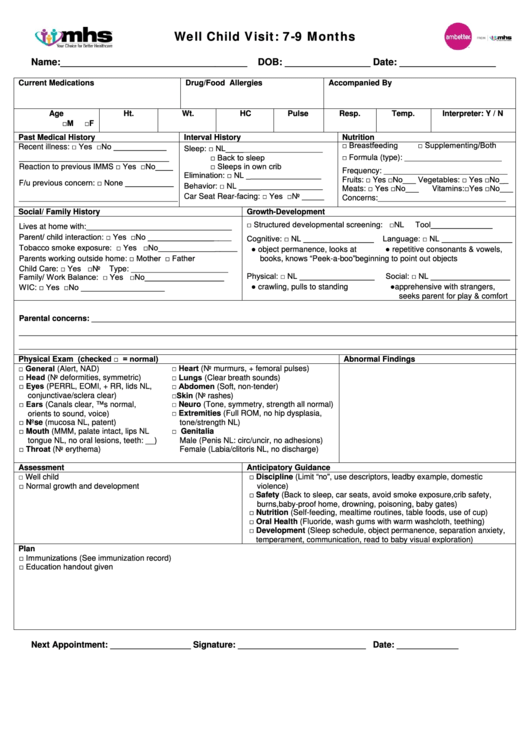
Well Child Visit: 7-9 Months
Name: ___________________________________
DOB: ________________ Date: __________________
Current Medications
Drug/Food Allergies
Accompanied By
Age
Ht.
Wt.
HC
Pulse
Resp.
Temp.
Interpreter: Y / N
□M
□F
Past Medical History
Interval History
Nutrition
Recent illness: □ Yes □No ____________
□ Breastfeeding
□ Supplementing/Both
Sleep: □ NL______________________
□ Formula (type): ______________________
□ Back to sleep
__________________________________
Reaction to previous IMMS □ Yes □No____
□ Sleeps in own crib
Frequency: ____________________________
Elimination: □ NL _________________
Fruits: □ Yes □No___ Vegetables: □ Yes □No__
F/u previous concern: □ None ___________
Behavior: □ NL ___________________
Meats: □ Yes □No___
Vitamins:□Yes □No___
Car Seat Rear-facing: □ Yes □No _____
Concerns:_____________________________
____________________________________
Social / Family History
Growth-Development
□ Structured developmental screening: □NL
Tool______________
Lives at home with:_________________________________
Parent/ child interaction: □ Yes □No ___________________
Cognitive: □ NL ________________
Language: □ NL ________________
Tobacco smoke exposure: □ Yes □No__________________
● object permanence, looks at
● repetitive consonants & vowels,
Parents working outside home: □ Mother
□ Father
books, knows “Peek-a-boo”
beginning to point out objects
Child Care: □ Yes □No
Type: ______________________
Physical: □ NL _________________
Social: □ NL __________________
Family/ Work Balance: □ Yes □No__________________
● crawling, pulls to standing
● apprehensive with strangers,
WIC: □ Yes □No ___________________
seeks parent for play & comfort
Parental concerns: ________________________________________________________________________________________________
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
Physical Exam (checked □ = normal)
Abnormal Findings
□ General (Alert, NAD)
□ Heart (No murmurs, + femoral pulses)
□ Head (No deformities, symmetric)
□ Lungs (Clear breath sounds)
□ Eyes (PERRL, EOMI, + RR, lids NL,
□ Abdomen (Soft, non-tender)
□Skin (No rashes)
conjunctivae/sclera clear)
□ Ears (Canals clear, TMs normal,
□ Neuro (Tone, symmetry, strength all normal)
□ Extremities (Full ROM, no hip dysplasia,
orients to sound, voice)
□ Nose (mucosa NL, patent)
tone/strength NL)
□ Mouth (MMM, palate intact, lips NL
□ Genitalia
tongue NL, no oral lesions, teeth: __)
Male (Penis NL: circ/uncir, no adhesions)
□ Throat (No erythema)
Female (Labia/clitoris NL, no discharge)
Assessment
Anticipatory Guidance
□ Well child
□ Discipline (Limit “no", use descriptors, lead by example, domestic
□ Normal growth and development
violence)
□ Safety (Back to sleep, car seats, avoid smoke exposure, crib safety,
burns, baby-proof home, drowning, poisoning, baby gates)
□ Nutrition (Self-feeding, mealtime routines, table foods, use of cup)
□ Oral Health (Fluoride, wash gums with warm washcloth, teething)
□ Development (Sleep schedule, object permanence, separation anxiety,
temperament, communication, read to baby visual exploration)
Plan
□ Immunizations (See immunization record)
□ Education handout given
Next Appointment: _________________ Signature: ___________________________ Date: _____________
1014.QI.P.FO 10/14
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1








