Express Scripts Claim Form
Download a blank fillable Express Scripts Claim Form in PDF format just by clicking the "DOWNLOAD PDF" button.
Open the file in any PDF-viewing software. Adobe Reader or any alternative for Windows or MacOS are required to access and complete fillable content.
Complete Express Scripts Claim Form with your personal data - all interactive fields are highlighted in places where you should type, access drop-down lists or select multiple-choice options.
Some fillable PDF-files have the option of saving the completed form that contains your own data for later use or sending it out straight away.
ADVERTISEMENT
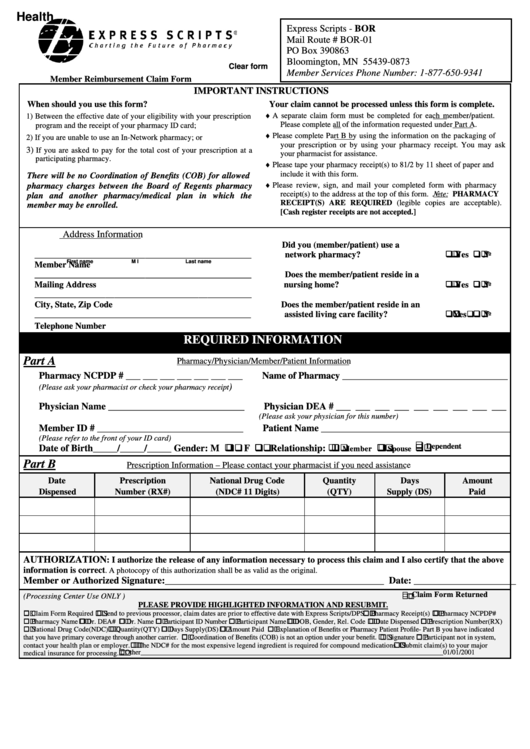
Health
Express Scripts - BOR
Mail Route # BOR-01
PO Box 390863
Bloomington, MN 55439-0873
Clear form
Member Services Phone Number: 1-877-650-9341
Member Reimbursement Claim Form
IMPORTANT INSTRUCTIONS
When should you use this form?
Your claim cannot be processed unless this form is complete.
♦
A separate claim form must be completed for each member/patient.
1) Between the effective date of your eligibility with your prescription
Please complete all of the information requested under Part A.
program and the receipt of your pharmacy ID card;
♦
Please complete Part B by using the information on the packaging of
2) If you are unable to use an In-Network pharmacy; or
your prescription or by using your pharmacy receipt. You may ask
3)
If you are asked to pay for the total cost of your prescription at a
your pharmacist for assistance.
participating pharmacy.
♦
Please tape your pharmacy receipt(s) to 81/2 by 11 sheet of paper and
include it with this form.
There will be no Coordination of Benefits (COB) for allowed
♦
Please review, sign, and mail your completed form with pharmacy
pharmacy charges between the Board of Regents pharmacy
receipt(s) to the address at the top of this form. Note: PHARMACY
plan and another pharmacy/medical plan in which the
RECEIPT(S) ARE REQUIRED (legible copies are acceptable).
member may be enrolled.
[Cash register receipts are not accepted.]
Address Information
Did you (member/patient) use a
! ! ! ! Yes ! ! ! ! No
_________________________________________________
network pharmacy?
First name
M I
Last name
Member Name
_________________________________________________
Does the member/patient reside in a
! ! ! ! Yes ! ! ! ! No
Mailing Address
nursing home?
_________________________________________________
City, State, Zip Code
Does the member/patient reside in an
! ! ! ! Yes ! ! ! ! No
_________________________________________________
assisted living care facility?
Telephone Number
REQUIRED INFORMATION
Part A
Pharmacy/Physician/Member/Patient Information
Pharmacy NCPDP # ___ ___ ___ ___ ___ ___ ___
Name of Pharmacy __________________________________
)
(Please ask your pharmacist or check your pharmacy receipt
Physician Name ____________________________
Physician DEA # ___ ___ ___ ___ ___ ___ ___ ___ ___
(Please ask your physician for this number)
Member ID # ______________________________
Patient Name _______________________________________
(Please refer to the front of your ID card)
Date of Birth_____/_____/_____ Gender: M ! ! ! ! F ! ! ! !
Relationship: ! ! ! !
! ! ! !
! ! ! !
Member
Spouse
Dependent
Part B
Prescription Information – Please contact your pharmacist if you need assistance
Date
Prescription
National Drug Code
Quantity
Days
Amount
Dispensed
Number (RX#)
(NDC# 11 Digits)
(QTY)
Supply (DS)
Paid
AUTHORIZATION
: I authorize the release of any information necessary to process this claim and I also certify that the above
information is correct
. A photocopy of this authorization shall be as valid as the original.
Member or Authorized Signature:_____________________________________________ Date: _____________________
" " " "
(Processing Center Use ONLY )
Claim Form Returned
PLEASE PROVIDE HIGHLIGHTED INFORMATION AND RESUBMIT.
" " " " Claim Form Required " " " " Send to previous processor, claim dates are prior to effective date with Express Scripts/DPS. " " " " Pharmacy Receipt(s) " " " " Pharmacy NCPDP#
" " " " Pharmacy Name " " " " Dr. DEA# " " " " Dr. Name " " " " Participant ID Number " " " " Participant Name " " " " DOB, Gender, Rel. Code " " " " Date Dispensed " " " " Prescription Number(RX)
" " " " National Drug Code(NDC) " " " " Quantity(QTY) " " " " Days Supply(DS) " " " " Amount Paid " " " " Explanation of Benefits or Pharmacy Patient Profile- Part B you have indicated
that you have primary coverage through another carrier. " " " " Coordination of Benefits (COB) is not an option under your benefit. " " " " Signature " " " " Participant not in system,
contact your health plan or employer. " " " " The NDC# for the most expensive legend ingredient is required for compound medications. " " " " Submit claim(s) to your major
medical insurance for processing. " " " " Other_______________________________________________________________________________________01/01/2001
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1








