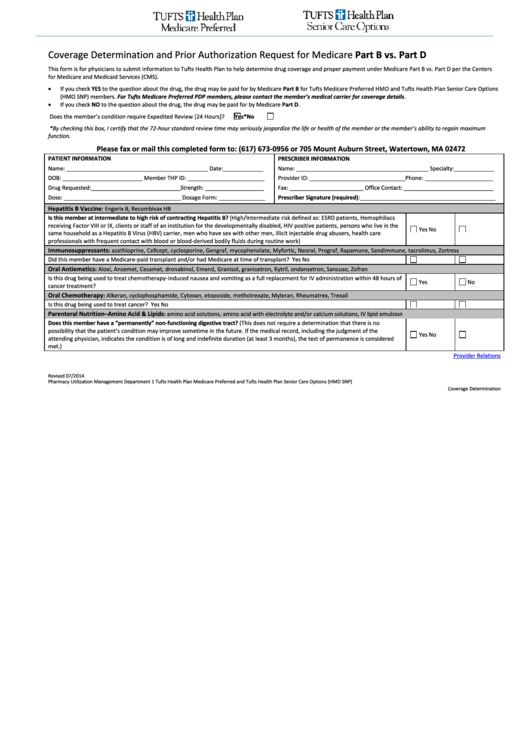
Coverage Determination and Prior Authorization Request for Medicare Part B vs. Part D
This form is for physicians to submit information to Tufts Health Plan to help determine drug coverage and proper payment under Medicare Part B vs. Part D per the Centers
for Medicare and Medicaid Services (CMS).
•
If you check YES to the question about the drug, the drug may be paid for by Medicare Part B for Tufts Medicare Preferred HMO and Tufts Health Plan Senior Care Options
(HMO SNP) members. For Tufts Medicare Preferred PDP members, please contact the member’s medical carrier for coverage details.
•
If you check NO to the question about the drug, the drug may be paid for by Medicare Part D.
Yes*
No
Does the member’s condition require Expedited Review [24 Hours]?
*By checking this box, I certify that the 72-hour standard review time may seriously jeopardize the life or health of the member or the member’s ability to regain maximum
function.
Please fax or mail this completed form to: (617) 673-0956 or 705 Mount Auburn Street, Watertown, MA 02472
PATIENT INFORMATION
PRESCRIBER INFORMATION
Name: ______________________________________________ Date:_____________
Name: ___________________________________________ Specialty:_____________
DOB: __________________________ Member THP ID: _________________________
Provider ID: _______________________________ Phone: ______________________
Drug Requested:_____________________________ Strength: ___________________
Fax: ________________________ Office Contact: _____________________________
Dose: ______________________________________ Dosage Form: _______________
Prescriber Signature (required):____________________________________________
Hepatitis B Vaccine : Engerix B, Recombivax HB
Is this member at intermediate to high risk of contracting Hepatitis B? (High/Intermediate risk defined as: ESRD patients, Hemophiliacs
receiving Factor VIII or IX, clients or staff of an institution for the developmentally disabled, HIV positive patients, persons who live in the
Yes
No
same household as a Hepatitis B Virus (HBV) carrier, men who have sex with other men, illicit injectable drug abusers, health care
professionals with frequent contact with blood or blood-derived bodily fluids during routine work)
Immunosuppressants : azathioprine, Cellcept, cyclosporine, Gengraf, mycophenolate, Myfortic, Neoral, Prograf, Rapamune, Sandimmune, tacrolimus, Zortress
Did this member have a Medicare-paid transplant and/or had Medicare at time of transplant?
Yes
No
Oral Antiemetics : Aloxi, Anzemet, Cesamet, dronabinol, Emend, Granisol, granisetron, Kytril, ondansetron, Sancuso, Zofran
Is this drug being used to treat chemotherapy-induced nausea and vomiting as a full replacement for IV administration within 48 hours of
Yes
No
cancer treatment?
Oral Chemotherapy : Alkeran, cyclophosphamide, Cytoxan, etoposide, methotrexate, Myleran, Rheumatrex, Trexall
Is this drug being used to treat cancer?
Yes
No
Parenteral Nutrition–Amino Acid & Lipids : amino acid solutions, amino acid with electrolyte and/or calcium solutions, IV lipid emulsion
Does this member have a “permanently” non-functioning digestive tract? (This does not require a determination that there is no
possibility that the patient’s condition may improve sometime in the future. If the medical record, including the judgment of the
Yes
No
attending physician, indicates the condition is of long and indefinite duration (at least 3 months), the test of permanence is considered
met.)
Provider Relations
Revised 07/2014
Pharmacy Utilization Management Department
1
Tufts Health Plan Medicare Preferred and Tufts Health Plan Senior Care Options (HMO SNP)
Coverage Determination
 1
1