Form Dobicappcar - Health Care Provider Application To Appeal A Claims Determination
ADVERTISEMENT
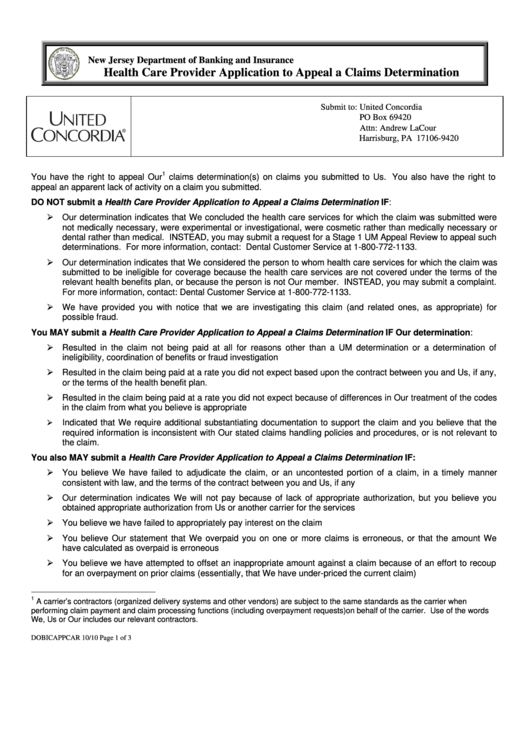
New Jersey Department of Banking and Insurance
Health Care Provider Application to Appeal a Claims Determination
Submit to: United Concordia
PO Box 69420
Attn: Andrew LaCour
Harrisburg, PA 17106-9420
1
You have the right to appeal Our
claims determination(s) on claims you submitted to Us. You also have the right to
appeal an apparent lack of activity on a claim you submitted.
DO NOT submit a Health Care Provider Application to Appeal a Claims Determination IF:
Our determination indicates that We concluded the health care services for which the claim was submitted were
not medically necessary, were experimental or investigational, were cosmetic rather than medically necessary or
dental rather than medical. INSTEAD, you may submit a request for a Stage 1 UM Appeal Review to appeal such
determinations. For more information, contact: Dental Customer Service at 1-800-772-1133.
Our determination indicates that We considered the person to whom health care services for which the claim was
submitted to be ineligible for coverage because the health care services are not covered under the terms of the
relevant health benefits plan, or because the person is not Our member. INSTEAD, you may submit a complaint.
For more information, contact: Dental Customer Service at 1-800-772-1133.
We have provided you with notice that we are investigating this claim (and related ones, as appropriate) for
possible fraud.
You MAY submit a Health Care Provider Application to Appeal a Claims Determination IF Our determination:
Resulted in the claim not being paid at all for reasons other than a UM determination or a determination of
ineligibility, coordination of benefits or fraud investigation
Resulted in the claim being paid at a rate you did not expect based upon the contract between you and Us, if any,
or the terms of the health benefit plan.
Resulted in the claim being paid at a rate you did not expect because of differences in Our treatment of the codes
in the claim from what you believe is appropriate
Indicated that We require additional substantiating documentation to support the claim and you believe that the
required information is inconsistent with Our stated claims handling policies and procedures, or is not relevant to
the claim.
You also MAY submit a Health Care Provider Application to Appeal a Claims Determination IF:
You believe We have failed to adjudicate the claim, or an uncontested portion of a claim, in a timely manner
consistent with law, and the terms of the contract between you and Us, if any
Our determination indicates We will not pay because of lack of appropriate authorization, but you believe you
obtained appropriate authorization from Us or another carrier for the services
You believe we have failed to appropriately pay interest on the claim
You believe Our statement that We overpaid you on one or more claims is erroneous, or that the amount We
have calculated as overpaid is erroneous
You believe we have attempted to offset an inappropriate amount against a claim because of an effort to recoup
for an overpayment on prior claims (essentially, that We have under-priced the current claim)
1
A carrier’s contractors (organized delivery systems and other vendors) are subject to the same standards as the carrier when
performing claim payment and claim processing functions (including overpayment requests)on behalf of the carrier. Use of the words
We, Us or Our includes our relevant contractors.
DOBICAPPCAR 10/10
Page 1 of 3
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2 3
3








