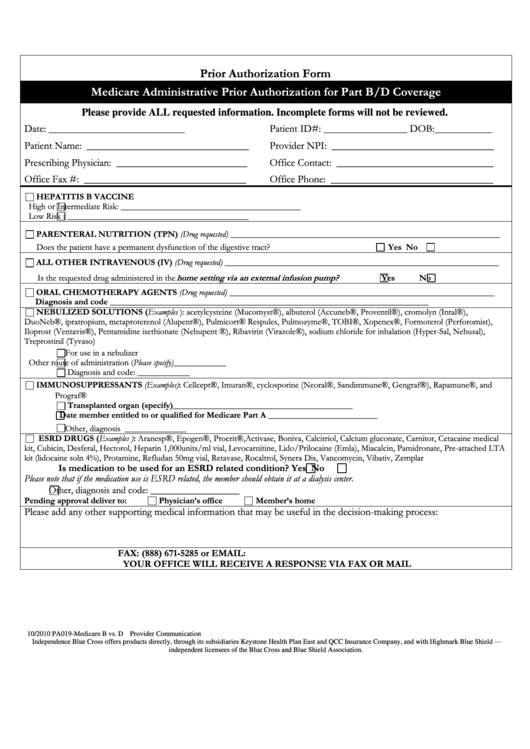
Medicare Administrative Prior Authorization For Part B/d Coverage
ADVERTISEMENT
Prior Authorization Form
Medicare Administrative Prior Authorization for Part B/D Coverage
Please provide ALL requested information. Incomplete forms will not be reviewed.
Date: __________________________
Patient ID#: ________________ DOB:___________
Patient Name: _______________________________
Provider NPI: _______________________________
Prescribing Physician: _________________________
Office Contact: ______________________________
Office Fax #: _______________________________
Office Phone: _______________________________
HEPATITIS B VACCINE
High or Intermediate Risk: _________________________________________
Low Risk : _________________________________________
PARENTERAL NUTRITION (TPN) (Drug requested) _____________________________________________________________
Does the patient have a permanent dysfunction of the digestive tract?
Yes
No
ALL OTHER INTRAVENOUS (IV) (Drug requested) ______________________________________________________________
Is the requested drug administered in the
home setting via an external infusion pump?
Yes
No
ORAL CHEMOTHERAPY AGENTS (Drug requested) ____________________________________________________________
Diagnosis and code ________________________________________________________________________
NEBULIZED SOLUTIONS (Examples ): acetylcysteine (Mucomyst®), albuterol (Accuneb®, Proventil®), cromolyn (Intal®),
DuoNeb®, ipratropium, metaproterenol (Alupent®), Pulmicort® Respules, Pulmozyme®, TOBI®, Xopenex®, Formoterol (Perforomist),
Iloprost (Ventavis®), Pentamidine isethionate (Nebupent ®), Ribavirin (Virazole®), sodium chloride for inhalation (Hyper-Sal, Nebusal),
Treprostinil (Tyvaso)
For use in a nebulizer
Other route of administration (Please specify)____________
Diagnosis and code: ____________
IMMUNOSUPPRESSANTS (Examples): Cellcept®, Imuran®, cyclosporine (Neoral®, Sandimmune®, Gengraf®), Rapamune®, and
Prograf®
Transplanted organ (specify)_________________________________________
Date member entitled to or qualified for Medicare Part A _________________________
Other, diagnosis ______________
ESRD DRUGS (Examples ): Aranesp®, Epogen®, Procrit®,Activase, Boniva, Calcitriol, Calcium gluconate, Carnitor, Cetacaine medical
kit, Cubicin, Desferal, Hectorol, Heparin 1,000units/ml vial, Levocarnitine, Lido/Prilocaine (Emla), Miacalcin, Pamidronate, Pre-attached LTA
kit (lidocaine soln 4%), Protamine, Refludan 50mg vial, Retavase, Rocaltrol, Synera Dis, Vancomycin, Vibativ, Zemplar
Is medication to be used for an ESRD related condition?
Yes
No
Please note that if the medication use is ESRD related, the member should obtain it at a dialysis center.
_________________
Other, diagnosis and code:
Pending approval deliver to:
Physician’s office
Member’s home
Please add any other supporting medical information that may be useful in the decision-making process:
FAX: (888) 671-5285 or EMAIL:
YOUR OFFICE WILL RECEIVE A RESPONSE VIA FAX OR MAIL
10/2010 PA019-Medicare B vs. D
Provider Communication
Independence Blue Cross offers products directly, through its subsidiaries Keystone Health Plan East and QCC Insurance Company, and with Highmark Blue Shield —
independent licensees of the Blue Cross and Blue Shield Association.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1