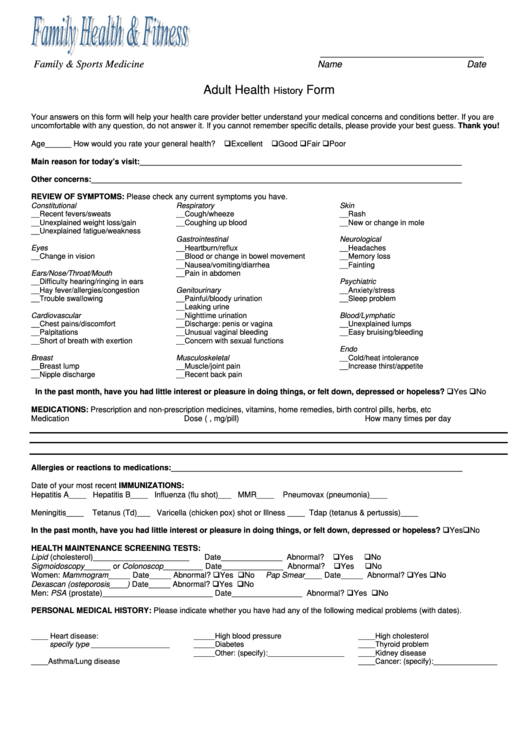
Adult Health History Form
ADVERTISEMENT
________________________________
Family & Sports Medicine
Name
Date
Adult Health History Form
Your answers on this form will help your health care provider better understand your medical concerns and conditions better. If you are
uncomfortable with any question, do not answer it. If you cannot remember specific details, please provide your best guess. Thank you!
Age______ How would you rate your general health?
Excellent
Good
Fair
Poor
Main reason for today’s visit:_________________________________________________________________________
Other concerns:____________________________________________________________________________________
REVIEW OF SYMPTOMS: Please check any current symptoms you have.
Constitutional
Respiratory
Skin
__Recent fevers/sweats
__Cough/wheeze
__Rash
__Unexplained weight loss/gain
__Coughing up blood
__New or change in mole
__Unexplained fatigue/weakness
Gastrointestinal
Neurological
Eyes
__Heartburn/reflux
__Headaches
__Change in vision
__Blood or change in bowel movement
__Memory loss
__Nausea/vomiting/diarrhea
__Fainting
Ears/Nose/Throat/Mouth
__Pain in abdomen
__Difficulty hearing/ringing in ears
Psychiatric
__Hay fever/allergies/congestion
Genitourinary
__Anxiety/stress
__Trouble swallowing
__Painful/bloody urination
__Sleep problem
__Leaking urine
Cardiovascular
__Nighttime urination
Blood/Lymphatic
__Chest pains/discomfort
__Discharge: penis or vagina
__Unexplained lumps
__Palpitations
__Unusual vaginal bleeding
__Easy bruising/bleeding
__Short of breath with exertion
__Concern with sexual functions
Endo
Breast
Musculoskeletal
__Cold/heat intolerance
__Breast lump
__Muscle/joint pain
__Increase thirst/appetite
__Nipple discharge
__Recent back pain
In the past month, have you had little interest or pleasure in doing things, or felt down, depressed or hopeless?
Yes
No
MEDICATIONS: Prescription and non-prescription medicines, vitamins, home remedies, birth control pills, herbs, etc
Medication
Dose (e.g., mg/pill)
How many times per day
Allergies or reactions to medications:__________________________________________________________________
Date of your most recent IMMUNIZATIONS:
Hepatitis A____ Hepatitis B____ Influenza (flu shot)___ MMR____
Pneumovax (pneumonia)____
Meningitis____
Tetanus (Td)___ Varicella (chicken pox) shot or Illness ____ Tdap (tetanus & pertussis)____
In the past month, have you had little interest or pleasure in doing things, or felt down, depressed or hopeless?
Yes No
HEALTH MAINTENANCE SCREENING TESTS:
Lipid (cholesterol)______________________
Date______________ Abnormal?
Yes
No
Sigmoidoscopy______ or Colonoscop_________ Date______________ Abnormal?
Yes
No
Women: Mammogram_____ Date_____ Abnormal?
Yes
No
Pap Smear____ Date_____ Abnormal?
Yes
No
Dexascan (osteporosis____) Date_____ Abnormal?
Yes
No
Men: PSA (prostate)_________________________ Date________________ Abnormal?
Yes
No
PERSONAL MEDICAL HISTORY: Please indicate whether you have had any of the following medical problems (with dates
).
____ Heart disease:
_____High blood pressure
____High cholesterol
specify type ___________________
_____Diabetes
____Thyroid problem
_____Other: (specify):__________________
____Kidney disease
____Asthma/Lung disease
____Cancer: (specify):_______________
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2