Health Information Questionnaire Form
ADVERTISEMENT
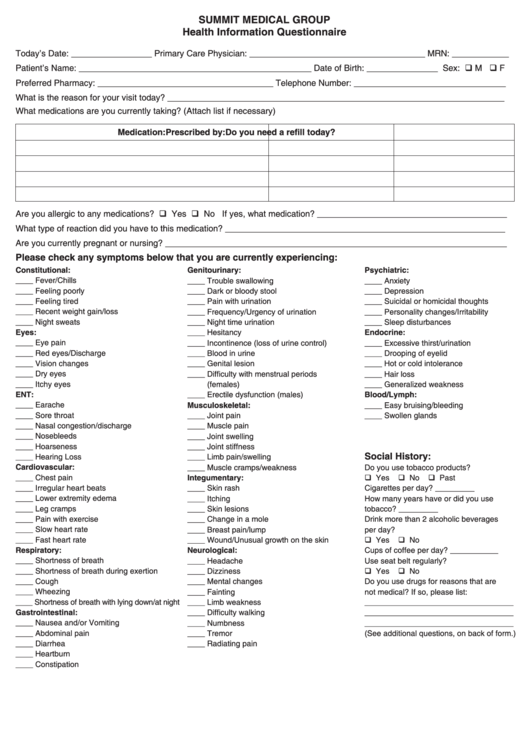
SUMMIT MEDICAL GROUP
Health Information Questionnaire
Today’s Date: _________________ Primary Care Physician: _____________________________________ MRN: ____________
Patient’s Name: _________________________________________________ Date of Birth: _______________ Sex: q M q F
Preferred Pharmacy: _____________________________________ Telephone Number: ________________________________
What is the reason for your visit today? _______________________________________________________________________
What medications are you currently taking? (Attach list if necessary)
Medication:
Prescribed by:
Do you need a refill today?
Are you allergic to any medications? q Yes q No If yes, what medication? ________________________________________
What type of reaction did you have to this medication? ___________________________________________________________
Are you currently pregnant or nursing? ________________________________________________________________________
Please check any symptoms below that you are currently experiencing:
Constitutional:
Genitourinary:
Psychiatric:
____ Fever/Chills
____ Trouble swallowing
____ Anxiety
____ Feeling poorly
____ Dark or bloody stool
____ Depression
____ Feeling tired
____ Pain with urination
____ Suicidal or homicidal thoughts
____ Recent weight gain/loss
____ Frequency/Urgency of urination
____ Personality changes/Irritability
____ Night sweats
____ Night time urination
____ Sleep disturbances
Eyes:
____ Hesitancy
Endocrine:
____ Eye pain
____ Incontinence (loss of urine control)
____ Excessive thirst/urination
____ Red eyes/Discharge
____ Blood in urine
____ Drooping of eyelid
____ Vision changes
____ Genital lesion
____ Hot or cold intolerance
____ Dry eyes
____ Difficulty with menstrual periods
____ Hair loss
____ Itchy eyes
(females)
____ Generalized weakness
ENT:
____ Erectile dysfunction (males)
Blood/Lymph:
____ Earache
Musculoskeletal:
____ Easy bruising/bleeding
____ Sore throat
____ Joint pain
____ Swollen glands
____ Nasal congestion/discharge
____ Muscle pain
____ Nosebleeds
____ Joint swelling
____ Hoarseness
____ Joint stiffness
Social History:
____ Hearing Loss
____ Limb pain/swelling
Cardiovascular:
____ Muscle cramps/weakness
Do you use tobacco products?
____ Chest pain
Integumentary:
q Yes
q No
q Past
____ Irregular heart beats
____ Skin rash
Cigarettes per day? _________
____ Lower extremity edema
____ Itching
How many years have or did you use
____ Leg cramps
____ Skin lesions
tobacco? _________
____ Pain with exercise
____ Change in a mole
Drink more than 2 alcoholic beverages
____ Slow heart rate
____ Breast pain/lump
per day?
____ Fast heart rate
____ Wound/Unusual growth on the skin
q Yes
q No
Respiratory:
Neurological:
Cups of coffee per day? ___________
____ Shortness of breath
____ Headache
Use seat belt regularly?
____ Shortness of breath during exertion
____ Dizziness
q Yes
q No
____ Cough
____ Mental changes
Do you use drugs for reasons that are
____ Wheezing
____ Fainting
not medical? If so, please list:
____ Shortness of breath with lying down/at night
____ Limb weakness
__________________________________
Gastrointestinal:
____ Difficulty walking
__________________________________
____ Nausea and/or Vomiting
____ Numbness
__________________________________
____ Abdominal pain
____ Tremor
(See additional questions, on back of form.)
____ Diarrhea
____ Radiating pain
____ Heartburn
____ Constipation
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2








