Form X16156r05 - Provider Claim Adjustment/status Check/appeal Form - Blue Cross Blue Shield Of Minnesota And Blue Plus Page 2
ADVERTISEMENT
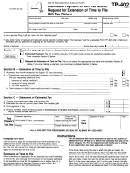
Provider Claim Adjustment / Status Check / Appeal Form Instructions
Blue Cross Blue Shield of Minnesota and Blue Plus
The general instructions are listed below. Please submit only one claim adjustment, status check or appeal
per page and mail with appropriate attachments to Blue Cross.
Field
Description
Contact Person
Provide the name of the person sending this request
Phone/Fax Number
List the office phone and fax numbers to contact you
Tax ID or Provider Number
Record your BCBSMN contracting provider number
NPI
Provide your National Provider Identifier number
Provider Name
Record the contracting provider business name
Provider Return Address
Provide the mailing address for correspondence regarding this request
Blue Cross Member ID#
Include any appropriate alpha prefix
Patient Name
Provide the patient’s name, as it may be different than the subscriber’s name
Patient Account
Provide the account number of your patient
Group Number
Provide the group number as it appears on the ID card
Claim Number
Attach a list of all claims impacted, if your appeal includes more than one claim
Note: Completion of all the above fields is required for submission of the request/appeal.
Claim Adjustment Request
•
When requesting a status check or claim adjustment, identify the reason for the inquiry and include detailed
information when necessary.
•
Include a letter from the doctor stating rationale for a diagnosis change.
•
Include medical records, chart notes and/or operative reports for the procedure or service if you are changing
the procedure code.
•
Please refer to the Provider Policy and Procedure Manual for instructions if you are adding a modifier to the
Procedure Code. [Some modifier changes can be adjusted, others must be appealed]
•
Include EOB/EOMB, designate Medicare, Workers’ Compensation or No Fault auto insurance, if another
carrier has paid on this claim.
Appeals
•
Incidental/Mutually Exclusive/Coding edit denial - Include a letter requesting review of codes that denied as
well as documentation such as office notes and/or operative reports.
•
Surgical Complications (Modifier 22) - Include chart notes, operative reports and/or a letter stating rationale
for the complication.
•
Medical Necessity - Include medical records and rationale for service performed.
•
Investigative - Include medical records and rationale for service performed.
•
Claim Denied for no Prior Authorization - Include medical records and rationale for service performed.
•
Incompatible Diagnosis - Include letter requesting review of codes that are denying as incompatible and
related notes.
•
DRG (Diagnostic Related Groups) /Category Code - Include rationale for questioning of payment.
•
Private Room - Include notes, doctor’s order and letter of medical necessity.
•
Allowed Amount - Include chart notes/invoice, NDC (National Drug Code) number and a letter to review
allowance for an unlisted code.
•
Timely Filing – See Provider Policy and Procedure Manual online at:
Status Checks: 651-662-8000 or 1-800-382-2000
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1 2
2