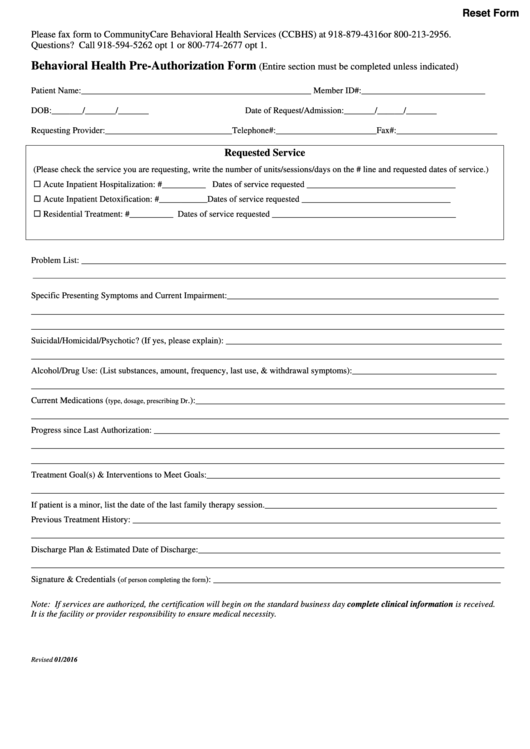
Reset Form
Please fax form to CommunityCare Behavioral Health Services (CCBHS) at 918-879-4316 or 800-213-2956.
Questions? Call 918-594-5262 opt 1 or 800-774-2677 opt 1.
Behavioral Health Pre-Authorization Form
(Entire section must be completed unless indicated)
Patient Name:____________________________________________________ Member ID#:____________________________
DOB:_______/_______/_______
Date of Request/Admission:_______/______/_______
Requesting Provider:_____________________________Telephone#:_______________________Fax#:_______________________
Requested Service
(Please check the service you are requesting, write the number of units/sessions/days on the # line and requested dates of service.)
Acute Inpatient Hospitalization: #__________ Dates of service requested __________________________________
Acute Inpatient Detoxification: #___________ Dates of service requested __________________________________
Residential Treatment: #__________ Dates of service requested __________________________________________
Problem List: ________________________________________________________________________________________________
______________________________________________________________________________________________________________________________________
Specific Presenting Symptoms and Current Impairment:______________________________________________________________
___________________________________________________________________________________________________________
___________________________________________________________________________________________________________
Suicidal/Homicidal/Psychotic? (If yes, please explain): _______________________________________________________________
___________________________________________________________________________________________________________
Alcohol/Drug Use: (List substances, amount, frequency, last use, & withdrawal symptoms):_________________________________
___________________________________________________________________________________________________________
Current Medications (
.):______________________________________________________________________
type, dosage, prescribing Dr
____________________________________________________________________________________________________________
Progress since Last Authorization: _______________________________________________________________________________
___________________________________________________________________________________________________________
___________________________________________________________________________________________________________
Treatment Goal(s) & Interventions to Meet Goals:___________________________________________________________________
___________________________________________________________________________________________________________
If patient is a minor, list the date of the last family therapy session._____________________________________________________
Previous Treatment History: ____________________________________________________________________________________
___________________________________________________________________________________________________________
Discharge Plan & Estimated Date of Discharge:_____________________________________________________________________
___________________________________________________________________________________________________________
Signature & Credentials (
): _________________________________________________________________
of person completing the form
Note: If services are authorized, the certification will begin on the standard business day complete clinical information is received.
It is the facility or provider responsibility to ensure medical necessity.
Revised 01/2016
 1
1