Request For Redetermination Of Medicare Prescription Drug Denial - Idaho Blue Cross
ADVERTISEMENT
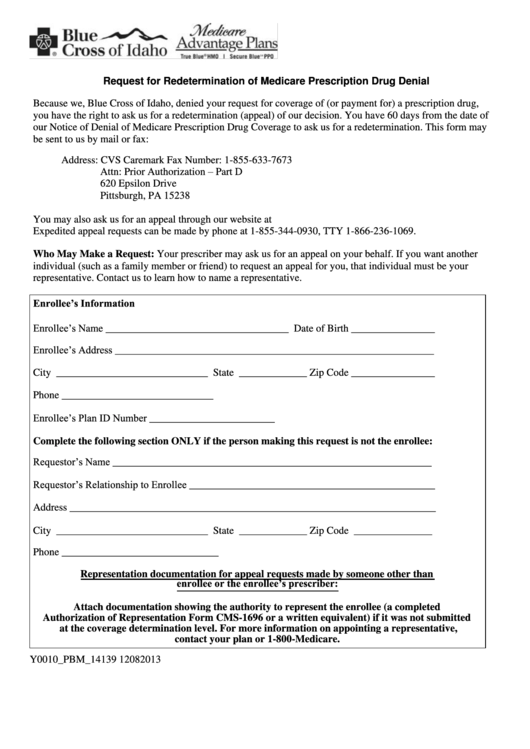
Request for Redetermination of Medicare Prescription Drug Denial
Because we, Blue Cross of Idaho, denied your request for coverage of (or payment for) a prescription drug,
you have the right to ask us for a redetermination (appeal) of our decision. You have 60 days from the date of
our Notice of Denial of Medicare Prescription Drug Coverage to ask us for a redetermination. This form may
be sent to us by mail or fax:
Address: CVS Caremark
Fax Number: 1-855-633-7673
Attn: Prior Authorization – Part D
620 Epsilon Drive
Pittsburgh, PA 15238
You may also ask us for an appeal through our website at
Expedited appeal requests can be made by phone at 1-855-344-0930, TTY 1-866-236-1069.
Who May Make a Request: Your prescriber may ask us for an appeal on your behalf. If you want another
individual (such as a family member or friend) to request an appeal for you, that individual must be your
representative. Contact us to learn how to name a representative.
Enrollee’s Information
Enrollee’s Name ___________________________________ Date of Birth ________________
Enrollee’s Address _____________________________________________________________
City _____________________________ State _____________ Zip Code ________________
Phone _____________________________
Enrollee’s Plan ID Number ________________________
Complete the following section ONLY if the person making this request is not the enrollee:
Requestor’s Name _____________________________________________________________
Requestor’s Relationship to Enrollee _______________________________________________
Address ______________________________________________________________________
City _____________________________ State _____________ Zip Code _______________
Phone ______________________________
Representation documentation for appeal requests made by someone other than
enrollee or the enrollee’s prescriber:
Attach documentation showing the authority to represent the enrollee (a completed
Authorization of Representation Form CMS-1696 or a written equivalent) if it was not submitted
at the coverage determination level. For more information on appointing a representative,
contact your plan or 1-800-Medicare.
Y0010_PBM_14139 12082013
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1 2
2








