Filing Instructions For The 2015 Mlr Reporting Year - Centers For Medicare & Medicaid Services (Cms) Page 27
ADVERTISEMENT
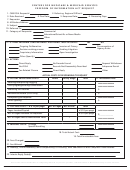
Instructions for MLR Annual Reporting Form − Part 2
(Premium and Claims)
These MLR Form Filing Instructions only apply to the 2015 MLR reporting year and its reporting
requirements. These Filing Instructions will be revised to reflect changes that apply to the filing years
subsequent to 2015.
In addition to the instructions below, the General Instructions and Column Definitions at the beginning of
these Filing Instructions apply to Part 2. The General Instructions and Column Definitions include
instructions regarding reporting of reinsurance, deferred business, individual business through an
association, employer business through a group trust or MEWA, group coverage in multiple States, and
dual contract group health coverage.
Please note that the MLR Form and Filing Instructions implement the requirements of 45 CFR Part 158
and are not identical to the definitions or instructions of the NAIC’s SHCE.
Section 1 – Health Premiums Earned
Earned premium means all monies paid by a policyholder or subscriber as a condition of receiving
coverage from the issuer, including any fees or other contributions associated with the health plan and
reported on a direct basis. Include advance payments of the premium tax credit. Any amounts for ACA
fees collected in advance of the MLR reporting year in which the fee is payable must not be reported as
unearned premium.
Line 1.1 – Direct premium written
12/31 Column – report amount as of 12/31 of the MLR reporting year, as reported to the
regulatory authority in the issuer’s State of domicile or as filed on the NAIC SHCE filing
for the MLR reporting year.
3/31 Column (premium for coverage in MLR reporting year only) – report premium collected
from 1/01 of the MLR reporting year through 3/31 of the year following the MLR
reporting year for coverage in the MLR reporting year only, plus uncollected (due and
unpaid) premium for coverage in the MLR reporting year only as of 3/31 of the year
following the MLR reporting year. Premium should reflect retroactive eligibility
adjustments related to coverage in the MLR reporting year.
PLEASE NOTE: This methodology differs from NAIC SHCE methodology. However,
issuers may choose to report amounts on the same basis as in the 12/31 columns, except
that risk adjustment amounts must not be reflected in the 3/31 columns.
Premium should include all amounts collected toward ACA fees, regardless of whether the
fees were included in premium or billed as a separate line item.
26
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2 3
3 4
4 5
5 6
6 7
7 8
8 9
9 10
10 11
11 12
12 13
13 14
14 15
15 16
16 17
17 18
18 19
19 20
20 21
21 22
22 23
23 24
24 25
25 26
26 27
27 28
28 29
29 30
30 31
31 32
32 33
33 34
34 35
35 36
36 37
37 38
38 39
39 40
40 41
41 42
42 43
43 44
44 45
45 46
46 47
47 48
48 49
49 50
50 51
51 52
52 53
53 54
54 55
55 56
56 57
57