Form Webpks-0034-16 - Reimbursement Reconsideration - Submission Form
ADVERTISEMENT
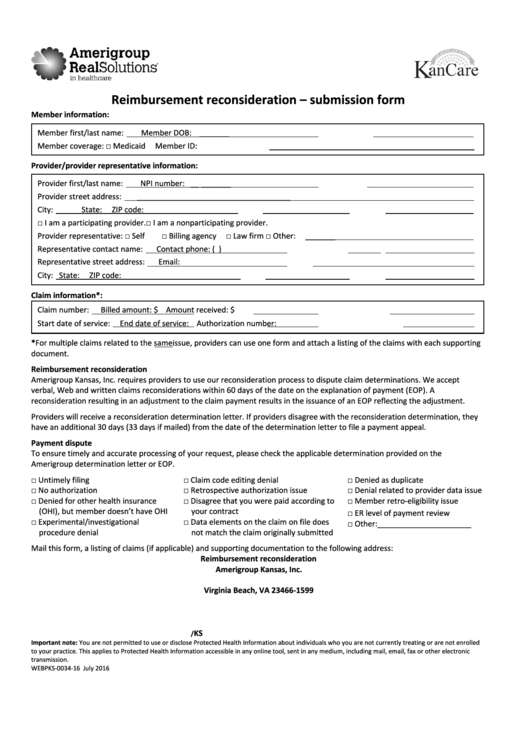
Reimbursement reconsideration – submission form
Member information:
Member first/last name:
Member DOB:
_______
Member coverage:
□ Medicaid
Member ID:
Provider/provider representative information:
Provider first/last name:
NPI number:
__
_______
Provider street address:
____________________________________
City:
___ State:
ZIP code:
_______
□ I am a participating provider.
□ I am a nonparticipating provider.
Provider representative: □ Self
□ Billing agency
□ Law firm
□ Other:
_______
Representative contact name:
Contact phone: (
)
Representative street address:
Email:
City:
State:
ZIP code:
Claim information*:
Claim number:
Billed amount: $
Amount received: $
Start date of service:
End date of service:
Authorization number:
*For multiple claims related to the same issue, providers can use one form and attach a listing of the claims with each supporting
document.
Reimbursement reconsideration
Amerigroup Kansas, Inc. requires providers to use our reconsideration process to dispute claim determinations. We accept
verbal, Web and written claims reconsiderations within 60 days of the date on the explanation of payment (EOP). A
reconsideration resulting in an adjustment to the claim payment results in the issuance of an EOP reflecting the adjustment.
Providers will receive a reconsideration determination letter. If providers disagree with the reconsideration determination, they
have an additional 30 days (33 days if mailed) from the date of the determination letter to file a payment appeal.
Payment dispute
To ensure timely and accurate processing of your request, please check the applicable determination provided on the
Amerigroup determination letter or EOP.
□ Untimely filing
□ Claim code editing denial
□ Denied as duplicate
□ No authorization
□ Retrospective authorization issue
□ Denial related to provider data issue
□ Denied for other health insurance
□ Disagree that you were paid according to
□ Member retro-eligibility issue
(OHI), but member doesn’t have OHI
your contract
□ ER level of payment review
□ Experimental/investigational
□ Data elements on the claim on file does
□ Other:______________________
procedure denial
not match the claim originally submitted
Mail this form, a listing of claims (if applicable) and supporting documentation to the following address:
Reimbursement reconsideration
Amerigroup Kansas, Inc.
P.O. Box 61599
Virginia Beach, VA 23466-1599
KS
/
Important note: You are not permitted to use or disclose Protected Health Information about individuals who you are not currently treating or are not enrolled
to your practice. This applies to Protected Health Information accessible in any online tool, sent in any medium, including mail, email, fax or other electronic
transmission.
WEBPKS-0034-16
July 2016
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1