Form Mc 1054 - Share-Of-Cost Medi-Cal Provider Letter
ADVERTISEMENT
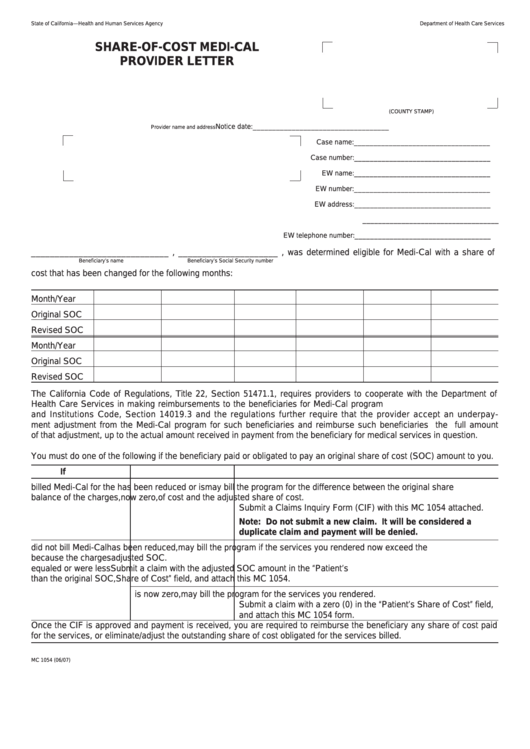
State of California—Health and Human Services Agency
Department of Health Care Services
SHARE-OF-COST MEDI-CAL
PROVIDER LETTER
(COUNTY STAMP)
Notice date:
___________________________________
Provider name and address
Case name:
___________________________________
Case number:
___________________________________
EW name:
___________________________________
EW number:
___________________________________
EW address:
___________________________________
___________________________________
EW telephone number:
___________________________________
_____________________________ , _____________________ , was determined eligible for Medi-Cal with a share of
Beneficiary’s name
Beneficiary’s Social Security number
cost that has been changed for the following months:
Month/Year
Original SOC
Revised SOC
Month/Year
Original SOC
Revised SOC
The California Code of Regulations, Title 22, Section 51471.1, requires providers to cooperate with the Department of
Health Care Services in making reimbursements to the beneficiaries for Medi-Cal program underpayments. The Welfare
and Institutions Code, Section 14019.3 and the regulations further require that the provider accept an underpay-
ment adjustment from the Medi-Cal program for such beneficiaries and reimburse such beneficiaries the full amount
of that adjustment, up to the actual amount received in payment from the beneficiary for medical services in question.
You must do one of the following if the beneficiary paid or obligated to pay an original share of cost (SOC) amount to you.
If you...
And the share of cost...
Then you...
billed Medi-Cal for the
has been reduced or is
may bill the program for the difference between the original share
balance of the charges,
now zero,
of cost and the adjusted share of cost.
Submit a Claims Inquiry Form (CIF) with this MC 1054 attached.
Note: Do not submit a new claim. It will be considered a
duplicate claim and payment will be denied.
did not bill Medi-Cal
has been reduced,
may bill the program if the services you rendered now exceed the
because the charges
adjusted SOC.
equaled or were less
Submit a claim with the adjusted SOC amount in the “Patient’s
than the original SOC,
Share of Cost” field, and attach this MC 1054.
is now zero,
may bill the program for the services you rendered.
Submit a claim with a zero (0) in the “Patient’s Share of Cost” field,
and attach this MC 1054 form.
Once the CIF is approved and payment is received, you are required to reimburse the beneficiary any share of cost paid
for the services, or eliminate/adjust the outstanding share of cost obligated for the services billed.
MC 1054 (06/07)
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1








