Corrective Action Plan Template And Instructions
ADVERTISEMENT
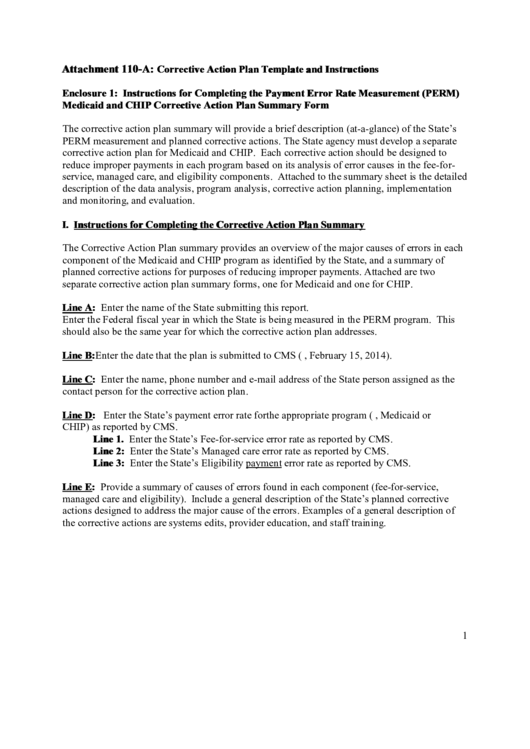
Attachment 110-A:
Corrective Action Plan Template and Instructions
Enclosure 1: Instructions for Completing the Payment Error Rate Measurement (PERM)
Medicaid and CHIP Corrective Action Plan Summary Form
The corrective action plan summary will provide a brief description (at-a-glance) of the State’s
PERM measurement and planned corrective actions. The State agency must develop a separate
corrective action plan for Medicaid and CHIP. Each corrective action should be designed to
reduce improper payments in each program based on its analysis of error causes in the fee-for-
service, managed care, and eligibility components. Attached to the summary sheet is the detailed
description of the data analysis, program analysis, corrective action planning, implementation
and monitoring, and evaluation.
I. Instructions for Completing the Corrective Action Plan Summary
The Corrective Action Plan summary provides an overview of the major causes of errors in each
component of the Medicaid and CHIP program as identified by the State, and a summary of
planned corrective actions for purposes of reducing improper payments. Attached are two
separate corrective action plan summary forms, one for Medicaid and one for CHIP.
Line A: Enter the name of the State submitting this report.
Enter the Federal fiscal year in which the State is being measured in the PERM program. This
should also be the same year for which the corrective action plan addresses.
Line B: Enter the date that the plan is submitted to CMS (e.g., February 15, 2014).
Line C: Enter the name, phone number and e-mail address of the State person assigned as the
contact person for the corrective action plan.
Line D: Enter the State’s payment error rate for the appropriate program (i.e., Medicaid or
CHIP) as reported by CMS.
Line 1. Enter the State’s Fee-for-service error rate as reported by CMS.
Line 2: Enter the State’s Managed care error rate as reported by CMS.
Line 3: Enter the State’s Eligibility payment error rate as reported by CMS.
Line E: Provide a summary of causes of errors found in each component (fee-for-service,
managed care and eligibility). Include a general description of the State’s planned corrective
actions designed to address the major cause of the errors. Examples of a general description of
the corrective actions are systems edits, provider education, and staff training.
1
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1 2
2 3
3 4
4 5
5 6
6 7
7 8
8 9
9 10
10 11
11








