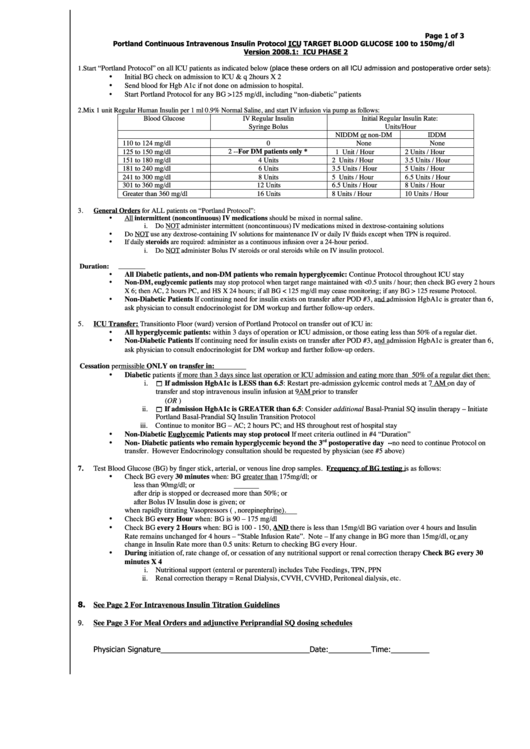
Insulin Dosage Chart
ADVERTISEMENT
Page 1 of 3
Portland Continuous Intravenous Insulin Protocol ICU TARGET BLOOD GLUCOSE 100 to 150mg/dl
Version 2008.1: ICU PHASE 2
(place these orders on all ICU admission and postoperative order sets):
“Portland Protocol” on all ICU patients as indicated below
1.
Start
•
Initial BG check on admission to ICU & q 2hours X 2
Send blood for Hgb A1c if not done on admission to hospital.
•
Start Portland Protocol for any BG >125 mg/dl, including “non-diabetic” patients
•
2.
Mix 1 unit Regular Human Insulin per 1 ml 0.9% Normal Saline, and start IV infusion via pump as follows:
Blood Glucose
IV Regular Insulin
Initial Regular Insulin Rate:
Syringe Bolus
Units/Hour
NIDDM or non-DM
IDDM
110 to 124 mg/dl
0
None
None
125 to 150 mg/dl
2 -- For DM patients only *
1 Unit / Hour
2 Units / Hour
151 to 180 mg/dl
4 Units
2 Units / Hour
3.5 Units / Hour
181 to 240 mg/dl
6 Units
3.5 Units / Hour
5 Units / Hour
241 to 300 mg/dl
8 Units
5 Units / Hour
6.5 Units / Hour
301 to 360 mg/dl
12 Units
6.5 Units / Hour
8 Units / Hour
Greater than 360 mg/dl
16 Units
8 Units / Hour
10 Units / Hour
3.
General Orders for ALL patients on “Portland Protocol”:
All intermittent (noncontinuous) IV medications should be mixed in normal saline.
•
i.
Do NOT administer intermittent (noncontinuous) IV medications mixed in dextrose-containing solutions
Do NOT use any dextrose-containing IV solutions for maintenance IV or daily IV fluids except when TPN is required.
•
•
If daily steroids are required: administer as a continuous infusion over a 24-hour period.
i.
Do NOT administer Bolus IV steroids or oral steroids while on IV insulin protocol.
4.
Protocol Duration:
All Diabetic patients, and non-DM patients who remain hyperglycemic: Continue Protocol throughout ICU stay
•
•
Non-DM, euglycemic patients may stop protocol when target range maintained with <0.5 units / hour; then check BG every 2 hours
X 6; then AC, 2 hours PC, and HS X 24 hours; if all BG < 125 mg/dl may cease monitoring; if any BG > 125 resume Protocol.
Non-Diabetic Patients If continuing need for insulin exists on transfer after POD #3, and admission HgbA1c is greater than 6,
•
ask physician to consult endocrinologist for DM workup and further follow-up orders.
5.
ICU Transfer: Transition to Floor (ward) version of Portland Protocol on transfer out of ICU in:
All hyperglycemic patients: within 3 days of operation or ICU admission, or those eating less
than 50% of a regular diet.
•
Non-Diabetic Patients If continuing need for insulin exists on transfer after POD #3, and admission HgbA1c is greater than 6,
•
ask physician to consult endocrinologist for DM workup and further follow-up orders.
6.
Protocol Cessation permissible ONLY on transfer in:
Diabetic patients if more than 3 days since last operation or ICU admission and eating more than 50% of a regular diet then:
•
If admission HgbA1c is LESS than 6.5: Restart pre-admission gylcemic control meds at 7 AM on day of
i.
transfer and stop intravenous insulin infusion at 9AM prior to transfer
(OR )
If admission HgbA1c is GREATER than 6.5: Consider additional Basal-Pranial SQ insulin therapy – Initiate
ii.
Portland Basal-Prandial SQ Insulin Transition Protocol
iii.
Continue to monitor BG – AC; 2 hours PC; and HS throughout rest of hospital stay
Non-Diabetic Euglycemic Patients may stop protocol If meet criteria outlined in #4 “Duration”
•
rd
•
Non- Diabetic patients who remain hyperglycemic beyond the 3
postoperative day -- no need to continue Protocol on
transfer. However Endocrinology consultation should be requested by physician (see #5 above)
7.
Test Blood Glucose (BG) by finger stick, arterial, or venous line drop samples. Frequency of BG testing is as follows:
Check BG every 30 minutes when: BG greater than 175mg/dl; or
•
less than 90mg/dl; or
after drip is stopped or decreased more than 50%; or
after Bolus IV Insulin dose is given; or
when rapidly titrating Vasopressors (e.g. epinephrine, norepinephrine).
•
Check BG every Hour when: BG is 90 – 175 mg/dl
Check BG every 2 Hours when: BG is 100 - 150, AND there is less than 15mg/dl BG variation over 4 hours and Insulin
•
Rate remains unchanged for 4 hours – “Stable Infusion Rate”. Note – If any change in BG more than 15mg/dl, or any
change in Insulin Rate more than 0.5 units: Return to checking BG every Hour.
During initiation of, rate change of, or cessation of any nutritional support or renal correction therapy Check BG every 30
•
minutes X 4
i.
Nutritional support (enteral or parenteral) includes Tube Feedings, TPN, PPN
ii.
Renal correction therapy = Renal Dialysis, CVVH, CVVHD, Peritoneal dialysis, etc.
8. See Page 2 For Intravenous Insulin Titration Guidelines
9.
See Page 3 For Meal Orders and adjunctive Periprandial SQ dosing schedules
Physician Signature___________________________________Date:__________Time:_________
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2 3
3