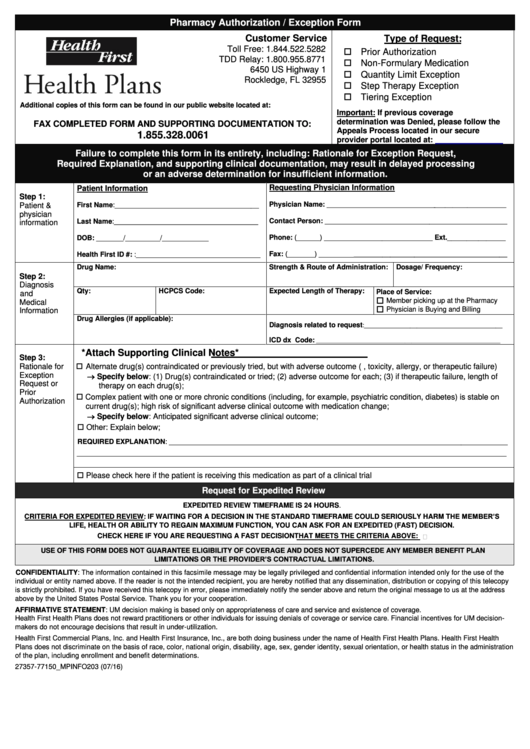
Pharmacy Authorization Exception Form - Health First
ADVERTISEMENT
Pharmacy Authorization / Exception Form
Customer Service
Type of Request:
Toll Free: 1.844.522.5282
Prior Authorization
TDD Relay: 1.800.955.8771
Non-Formulary Medication
6450 US Highway 1
Quantity Limit Exception
Rockledge, FL 32955
Step Therapy Exception
Tiering Exception
Additional copies of this form can be found in our public website located at:
Important: If previous coverage
determination was Denied, please follow the
FAX COMPLETED FORM AND SUPPORTING DOCUMENTATION TO:
Appeals Process located in our secure
1.855.328.0061
provider portal located at:
Failure to complete this form in its entirety, including: Rationale for Exception Request,
Required Explanation, and supporting clinical documentation, may result in delayed processing
or an adverse determination for insufficient information.
Requesting Physician Information
Patient Information
Step 1:
Physician Name: _______________________________________________
Patient &
First Name:_____________________________________
physician
Contact Person: _______________________________________________
Last Name:_____________________________________
information
Phone: (______) ____________________________ Ext._______________
DOB: _______/_________/____________
Fax: (_______) ________________________________________________
Health First ID #: :________________________________
Drug Name:
Strength & Route of Administration:
Dosage/ Frequency:
Step 2:
Diagnosis
Qty:
HCPCS Code:
Expected Length of Therapy:
Place of Service:
and
Member picking up at the Pharmacy
Medical
Physician is Buying and Billing
Information
Drug Allergies (if applicable):
Diagnosis related to request
:__________________________________________
ICD dx Code:
________________________________________________________
*Attach Supporting Clinical Notes*
Step 3:
Alternate drug(s) contraindicated or previously tried, but with adverse outcome (e.g., toxicity, allergy, or therapeutic failure)
Rationale for
Specify below: (1) Drug(s) contraindicated or tried; (2) adverse outcome for each; (3) if therapeutic failure, length of
Exception
Request or
therapy on each drug(s);
Prior
Complex patient with one or more chronic conditions (including, for example, psychiatric condition, diabetes) is stable on
Authorization
current drug(s); high risk of significant adverse clinical outcome with medication change;
Specify below: Anticipated significant adverse clinical outcome;
Other: Explain below;
REQUIRED EXPLANATION: _______________________________________________________________________________________
_______________________________________________________________________________________________________________
Please check here if the patient is receiving this medication as part of a clinical trial
Request for Expedited Review
EXPEDITED REVIEW TIMEFRAME IS 24 HOURS.
CRITERIA FOR EXPEDITED REVIEW: IF WAITING FOR A DECISION IN THE STANDARD TIMEFRAME COULD SERIOUSLY HARM THE MEMBER’S
LIFE, HEALTH OR ABILITY TO REGAIN MAXIMUM FUNCTION, YOU CAN ASK FOR AN EXPEDITED (FAST) DECISION.
CHECK HERE IF YOU ARE REQUESTING A FAST DECISION THAT MEETS THE CRITERIA ABOVE:
USE OF THIS FORM DOES NOT GUARANTEE ELIGIBILITY OF COVERAGE AND DOES NOT SUPERCEDE ANY MEMBER BENEFIT PLAN
LIMITATIONS OR THE PROVIDER’S CONTRACTUAL LIMITATIONS.
CONFIDENTIALITY: The information contained in this facsimile message may be legally privileged and confidential information intended only for the use of the
individual or entity named above. If the reader is not the intended recipient, you are hereby notified that any dissemination, distribution or copying of this telecopy
is strictly prohibited. If you have received this telecopy in error, please immediately notify the sender above and return the original message to us at the address
above by the United States Postal Service. Thank you for your cooperation.
AFFIRMATIVE STATEMENT: UM decision making is based only on appropriateness of care and service and existence of coverage.
Health First Health Plans does not reward practitioners or other individuals for issuing denials of coverage or service care. Financial incentives for UM decision-
makers do not encourage decisions that result in under-utilization.
Health First Commercial Plans, Inc. and Health First Insurance, Inc., are both doing business under the name of Health First Health Plans. Health First Health
Plans does not discriminate on the basis of race, color, national origin, disability, age, sex, gender identity, sexual orientation, or health status in the administration
of the plan, including enrollment and benefit determinations.
27357-77150_MPINFO203 (07/16)
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1