Texas Medicaid/CHIP Vendor Drug Program
Fee-For-Service Medicaid
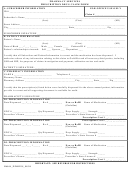
Retroactive Claim Form
About
The Vendor Drug Program utilizes the Retroactive Claim Form to assist pharmacy providers with an
expedited process for the payment of retroactive fee-for-service Medicaid claims.
Usage
The form is only for Medicaid clients with retroactive coverage and will be returned with no action taken if
used for other purposes.
The total number of pending claims, and the date of service of the oldest claim, must be included to determine
accurate certification and effective dates. Expect lengthened turnaround if this is not provided.
Please refer to Texas Administrative Code §354.1877 ( ) for information
pertaining to quantity limitations and refills:
Except for medications that may be too unstable to be dispensed as a one-month supply, the Health and Human
Services Commission requires that the same drug in the same strength be dispensed no more than once per month.
Claims with the same National Drug Code for service dates within the same month must be combined for one
billing per month. Claims that are not combined will not be paid.
Instructions
Please complete all fields in the Pharmacy and Client
For clients enrolled in fee-for-service Medicaid only.
information sections. Utilize the Pharmacy Comments field as needed. Return the form:
By fax:
512-491-1958
Attention: VDP Pharmacy Benefits Access
Response
If after our research the claims are approved for payment, and the number of pending claims is given, the
rejected claims will be paid. The completed form will be returned to the pharmacy within two weeks.
If the claims are not approved an explanation will be provided when the form is returned.
Rev. 10/2014
Page 1 of 2
File: vdp_ecm_retroc
 1
1 2
2