Form 9765- Oregon Health Plan Continuation Notice
ADVERTISEMENT
ABC
AB
Independent Licensees of the Blue Cross and Blue Shield Association
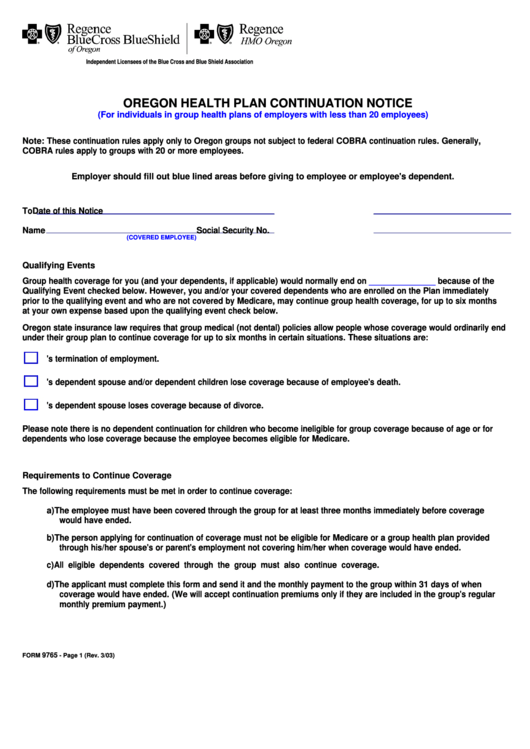
OREGON HEALTH PLAN CONTINUATION NOTICE
(For individuals in group health plans of employers with less than 20 employees)
Note: These continuation rules apply only to Oregon groups not subject to federal COBRA continuation rules. Generally,
COBRA rules apply to groups with 20 or more employees.
Employer should fill out blue lined areas before giving to employee or employee's dependent.
To
Date of this Notice
Name
Social Security No.
(COVERED EMPLOYEE)
Qualifying Events
Group health coverage for you (and your dependents, if applicable) would normally end on
______________
because of the
Qualifying Event checked below. However, you and/or your covered dependents who are enrolled on the Plan immediately
prior to the qualifying event and who are not covered by Medicare, may continue group health coverage, for up to six months
at your own expense based upon the qualifying event check below.
Oregon state insurance law requires that group medical (not dental) policies allow people whose coverage would ordinarily end
under their group plan to continue coverage for up to six months in certain situations. These situations are:
1. The employee's termination of employment.
2. The employee's dependent spouse and/or dependent children lose coverage because of employee's death.
3. The employee's dependent spouse loses coverage because of divorce.
Please note there is no dependent continuation for children who become ineligible for group coverage because of age or for
dependents who lose coverage because the employee becomes eligible for Medicare.
Requirements to Continue Coverage
The following requirements must be met in order to continue coverage:
a) The employee must have been covered through the group for at least three months immediately before coverage
would have ended.
b) The person applying for continuation of coverage must not be eligible for Medicare or a group health plan provided
through his/her spouse's or parent's employment not covering him/her when coverage would have ended.
c) All eligible dependents covered through the group must also continue coverage.
d) The applicant must complete this form and send it and the monthly payment to the group within 31 days of when
coverage would have ended. (We will accept continuation premiums only if they are included in the group's regular
monthly premium payment.)
9765
FORM
- Page 1 (Rev. 3/03)
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1 2
2 3
3 4
4








