Prior Authorization Requirements Exemption Request
ADVERTISEMENT
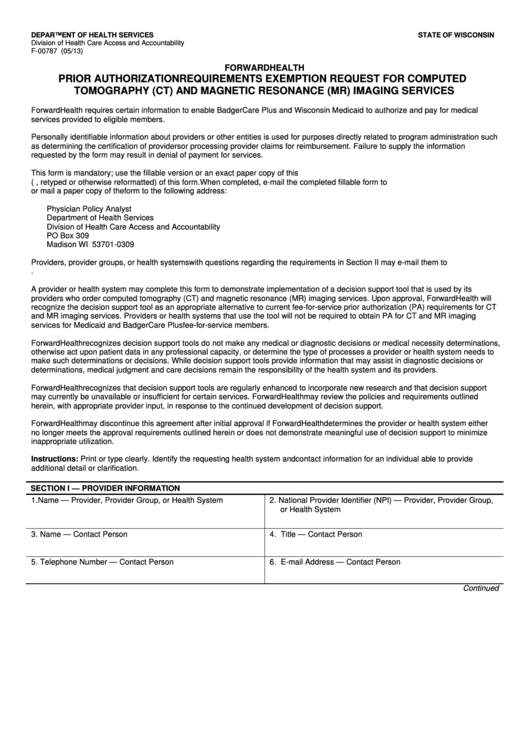
DEPARTMENT OF HEALTH SERVICES
STATE OF WISCONSIN
Division of Health Care Access and Accountability
F-00787 (05/13)
FORWARDHEALTH
PRIOR AUTHORIZATION REQUIREMENTS EXEMPTION REQUEST FOR COMPUTED
TOMOGRAPHY (CT) AND MAGNETIC RESONANCE (MR) IMAGING SERVICES
ForwardHealth requires certain information to enable BadgerCare Plus and Wisconsin Medicaid to authorize and pay for medical
services provided to eligible members.
Personally identifiable information about providers or other entities is used for purposes directly related to program administration such
as determining the certification of providers or processing provider claims for reimbursement. Failure to supply the information
requested by the form may result in denial of payment for services.
This form is mandatory; use the fillable version or an exact paper copy of this form. ForwardHealth will not accept alternate versions
(i.e., retyped or otherwise reformatted) of this form. When completed, e-mail the completed fillable form to
DHSPAExemption@wisconsin.gov or mail a paper copy of the form to the following address:
Physician Policy Analyst
Department of Health Services
Division of Health Care Access and Accountability
PO Box 309
Madison WI 53701-0309
Providers, provider groups, or health systems with questions regarding the requirements in Section II may e-mail them to
DHSPAExemption@wisconsin.gov.
A provider or health system may complete this form to demonstrate implementation of a decision support tool that is used by its
providers who order computed tomography (CT) and magnetic resonance (MR) imaging services. Upon approval, ForwardHealth will
recognize the decision support tool as an appropriate alternative to current fee-for-service prior authorization (PA) requirements for CT
and MR imaging services. Providers or health systems that use the tool will not be required to obtain PA for CT and MR imaging
services for Medicaid and BadgerCare Plus fee-for-service members.
ForwardHealth recognizes decision support tools do not make any medical or diagnostic decisions or medical necessity determinations,
otherwise act upon patient data in any professional capacity, or determine the type of processes a provider or health system needs to
make such determinations or decisions. While decision support tools provide information that may assist in diagnostic decisions or
determinations, medical judgment and care decisions remain the responsibility of the health system and its providers.
ForwardHealth recognizes that decision support tools are regularly enhanced to incorporate new research and that decision support
may currently be unavailable or insufficient for certain services. ForwardHealth may review the policies and requirements outlined
herein, with appropriate provider input, in response to the continued development of decision support.
ForwardHealth may discontinue this agreement after initial approval if ForwardHealth determines the provider or health system either
no longer meets the approval requirements outlined herein or does not demonstrate meaningful use of decision support to minimize
inappropriate utilization.
Instructions: Print or type clearly. Identify the requesting health system and contact information for an individual able to provide
additional detail or clarification.
SECTION I — PROVIDER INFORMATION
1. Name — Provider, Provider Group, or Health System
2. National Provider Identifier (NPI) — Provider, Provider Group,
or Health System
3. Name — Contact Person
4. Title — Contact Person
5. Telephone Number — Contact Person
6. E-mail Address — Contact Person
Continued
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2








