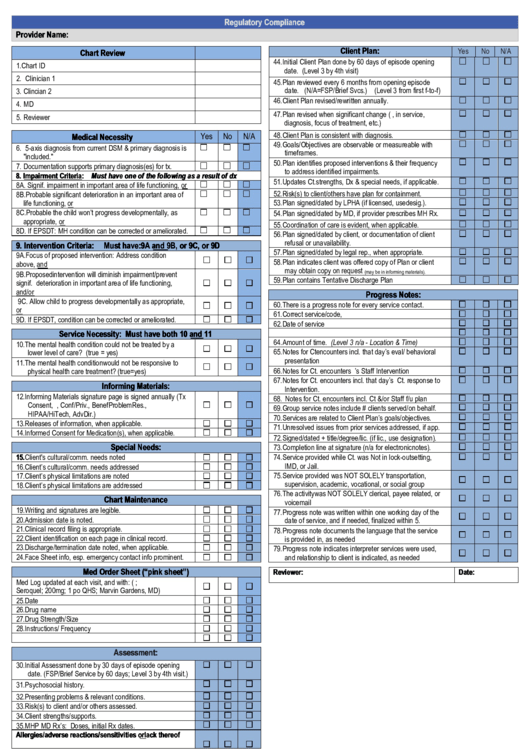
Regulatory Compliance
ADVERTISEMENT
Regulatory Compliance
Provider Name:
Client Plan:
Yes
No
N/A
Chart Review
44. Initial Client Plan done by 60 days of episode opening
1. Chart ID
date. (Level 3 by 4th visit)
2. Clinician 1
45. Plan reviewed every 6 months from opening episode
date. (N/A=FSP/Brief Svcs.) (Level 3 from first f-to-f)
3. Clincian 2
46. Client Plan revised/rewritten annually.
4. MD
47. Plan revised when significant change (e.g., in service,
5. Reviewer
diagnosis, focus of treatment, etc.)
48. Client Plan is consistent with diagnosis.
Medical Necessity
Yes
No
N/A
49. Goals/Objectives are observable or measureable with
6. 5-axis diagnosis from current DSM & primary diagnosis is
timeframes.
"included."
50. Plan identifies proposed interventions & their frequency
7. Documentation supports primary diagnosis(es) for tx.
to address identified impairments.
8. Impairment Criteria: Must have one of the following as a result of dx
51. Updates Ct. strengths, Dx & special needs, if applicable.
8A. Signif. impairment in important area of life functioning, or
52. Risk(s) to client/others have plan for containment.
8B. Probable significant deterioration in an important area of
53. Plan signed/dated by LPHA (if licensed, use desig.).
life functioning, or
8C. Probable the child won’t progress developmentally, as
54. Plan signed/dated by MD, if provider prescribes MH Rx.
appropriate, or
55. Coordination of care is evident, when applicable.
8D. If EPSDT: MH condition can be corrected or ameliorated.
56. Plan signed/dated by client, or documentation of client
refusal or unavailability.
9. Intervention Criteria:
Must have: 9A and 9B, or 9C, or 9D
57. Plan signed/dated by legal rep., when appropriate.
9A. Focus of proposed intervention: Address condition
58. Plan indicates client was offered copy of Plan or client
above, and
may obtain copy on request
9B. Proposed intervention will diminish impairment/prevent
(may be in informing materials).
59. Plan contains Tentative Discharge Plan
signif. deterioration in important area of life functioning,
and/or
Progress Notes:
9C. Allow child to progress developmentally as appropriate,
60. There is a progress note for every service contact.
or
61. Correct service/code,
9D. If EPSDT, condition can be corrected or ameliorated.
62. Date of service
63. Location
Service Necessity: Must have both 10 and 11
64. Amount of time. (Level 3 n/a - Location & Time)
10. The mental health condition could not be treated by a
65. Notes for Ct encounters incl. that day’s eval/ behavioral
lower level of care? (true = yes)
presentation
11. The mental health condition would not be responsive to
66. Notes for Ct. encounters incl.that day’s Staff Intervention
physical health care treatment? (true=yes)
67. Notes for Ct. encounters incl. that day’s Ct. response to
Informing Materials:
Intervention.
12. Informing Materials signature page is signed annually (Tx
68. Notes for Ct. encounters incl. Ct &/or Staff f/u plan
Consent, Free.Choice, Conf/Priv., BenefProblemRes.,
69. Group service notes include # clients served/on behalf.
HIPAA/HiTech, AdvDir.)
70. Services are related to Client Plan’s goals/objectives.
13. Releases of information, when applicable.
71. Unresolved issues from prior services addressed, if app.
14. Informed Consent for Medication(s), when applicable.
72. Signed/dated + title/degree/lic. (if lic., use designation).
Special Needs:
73. Completion line at signature (n/a for electronic notes).
15. Client's cultural/comm. needs noted
74. Service provided while Ct. was Not in lock-out setting,
IMD, or Jail.
16. Client’s cultural/comm. needs addressed
75. Service provided was NOT SOLELY transportation,
17. Client’s physical limitations are noted
supervision, academic, vocational, or social group
18. Client’s physical limitations are addressed
76. The activity was NOT SOLELY clerical, payee related, or
Chart Maintenance
voicemail
19. Writing and signatures are legible.
77. Progress note was written within one working day of the
20. Admission date is noted.
date of service, and if needed, finalized within 5.
21. Clinical record filing is appropriate.
78. Progress note documents the language that the service
22. Client identification on each page in clinical record.
is provided in, as needed
23. Discharge/termination date noted, when applicable.
79. Progress note indicates interpreter services were used,
24. Face Sheet info, esp. emergency contact info prominent.
and relationship to client is indicated, as needed
Med Order Sheet (“pink sheet”)
Reviewer:
Date:
Med Log updated at each visit, and with: (i.e. 4/8/10;
Seroquel; 200mg; 1 po QHS; Marvin Gardens, MD)
25. Date
26. Drug name
27. Drug Strength/Size
28. Instructions/ Frequency
29. Signatures/Initials
Assessment:
30. Initial Assessment done by 30 days of episode opening
date. (FSP/Brief Service by 60 days; Level 3 by 4th visit.)
31. Psychosocial history.
32. Presenting problems & relevant conditions.
33. Risk(s) to client and/or others assessed.
34. Client strengths/supports.
35. MHP MD Rx’s: Doses, initial Rx dates.
Allergies/adverse reactions/sensitivities or lack thereof
36. Noted in chart
Allergies/adverse reactions/sensitivities or lack thereof
37. Noted prominently on chart’s cover.
38. Relevant medical conditions/hx noted & updated.
39. Mental health history.
40. Relevant mental status exam (MSE).
41. Past/present use: Tobacco, alcohol, caffeine,
illicit/Rx/OTC drugs.
42. Youth: Pre/perinatal events & complete dev. hx.
43. Annual Community Functioning Evaluation (ACFE)
N/A for FSP/Brief Service Programs & Level 3)
Regulatory Compliance V.12-20-12
Update 12-20-12
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Education
 1
1








