Subscriber/member Enrollment Form Page 2
ADVERTISEMENT
ELECTION OF COVERAGE
I am enrolling for coverage for myself, my spouse and unmarried children under the age limit shown on the group schedule of benefits who are full time students
at an accredited educational institution and who are dependent on me and/or my spouse for support.
If I am required to contribute to the premium for my coverage, I hereby authorize my employer to deduct such contributions in advance from wages due me and
to remit same to HIP.
Any person who knowingly and with intent to defraud any insurance company or other person, files an application for insurance or statement of claim containing
any materially false information, or conceals for the purpose of misleading, information concerning any fact material thereto, commits a fraudulent insurance act, which
is a crime, and shall be subject to civil penalty not to exceed five thousand dollars and the stated value of the claim for each violation.
HIP PRIME POS and HIPaccess II applicants please note that your benefits are provided under two separate contracts: a HIP HMO contract issued by the Health
Insurance Plan of Greater New York, and a HIP PRIME POS and/or HIPaccess II contract issued by the HIP Insurance Company of New York. Both contracts will
end simultaneously if your HIP PRIME POS or HIPaccess II coverage ends.
The following paragraph pertains to small business groups only.
I understand that pre-existing conditions will not be covered during the first 12 months of my enrollment under my group’s contract. A pre-existing con-
dition is a condition (whether physical or mental) regardless of the cause of the condition, for which medical advice, diagnosis, care or treatment was recom-
mended by a duly licensed medical professional or received within the six (6) month period ending on the enrollment date. Except that, pregnancy is not
considered a pre-existing condition and genetic information may not be treated as a pre-existing condition in the absence of a diagnosis of the condition relat-
ed to such genetic information. HIP will credit the time I/we were covered by the previous policy, provided that the break in coverage under this plan does
not exceed sixty-three (63) days, exclusive of any waiting periods. I agree that after enrolled, I will upon request provide HIP and/or my medical group with
information on pre-existing conditions and any previous coverage I had. Subject to the applicable State and Federal laws pertaining to pre-existing conditions
and creditable coverage, benefits for pre-existing conditions may not be payable for up to twelve months from my effective date under my group’s contract.
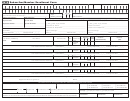
SECTION A
DOCUMENTATION BASED ON GROUP SIZE
(To be completed by
Group Type (Check One)
Benefits Administrator)
Sole Proprietorship
Association of
Small Group -
ACTION
or One Subscriber
Two or More
Less Than 50
Check (✔)One
Qualifying Event
Documentation Required
Group
Employees
Employees
New Hire or
For eligible employees who work more
Add Subscriber
than 20 hours weekly provide a recent
Change in Plan
Not Eligible
Copy of NYS45 showing this subscriber
as an employee or copy of Payroll docu-
mentation reflecting the date, employee’s
name and Social Security # or the
employee’s current year W4 form.
Add Spouse
Marriage
Marriage Certificate
Add Dependent
Birth
Birth Certificate or
Adoption
Formal Adoption Papers or
Court Approved Guardianship Papers
Add Spouse
Loss of Coverage
Add Dependent
Certificate of Creditable Coverage
Note: No Retroactive Enrollments will be allowed. Members must be enrolled within 30 days from the Qualifying Event.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1 2
2