Form Gc-7 - Aetna Medical Claiand Benefits Request Form
ADVERTISEMENT
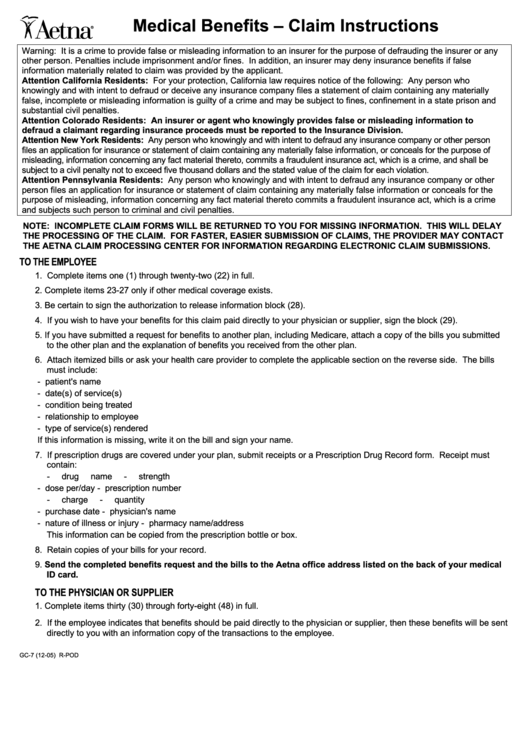
Medical Benefits – Claim Instructions
Warning: It is a crime to provide false or misleading information to an insurer for the purpose of defrauding the insurer or any
other person. Penalties include imprisonment and/or fines. In addition, an insurer may deny insurance benefits if false
information materially related to claim was provided by the applicant.
Attention California Residents: For your protection, California law requires notice of the following: Any person who
knowingly and with intent to defraud or deceive any insurance company files a statement of claim containing any materially
false, incomplete or misleading information is guilty of a crime and may be subject to fines, confinement in a state prison and
substantial civil penalties.
Attention Colorado Residents: An insurer or agent who knowingly provides false or misleading information to
defraud a claimant regarding insurance proceeds must be reported to the Insurance Division.
Attention New York Residents: Any person who knowingly and with intent to defraud any insurance company or other person
files an application for insurance or statement of claim containing any materially false information, or conceals for the purpose of
misleading, information concerning any fact material thereto, commits a fraudulent insurance act, which is a crime, and shall be
subject to a civil penalty not to exceed five thousand dollars and the stated value of the claim for each violation.
Attention Pennsylvania Residents: Any person who knowingly and with intent to defraud any insurance company or other
person files an application for insurance or statement of claim containing any materially false information or conceals for the
purpose of misleading, information concerning any fact material thereto commits a fraudulent insurance act, which is a crime
and subjects such person to criminal and civil penalties.
NOTE: INCOMPLETE CLAIM FORMS WILL BE RETURNED TO YOU FOR MISSING INFORMATION. THIS WILL DELAY
THE PROCESSING OF THE CLAIM. FOR FASTER, EASIER SUBMISSION OF CLAIMS, THE PROVIDER MAY CONTACT
THE AETNA CLAIM PROCESSING CENTER FOR INFORMATION REGARDING ELECTRONIC CLAIM SUBMISSIONS.
TO THE EMPLOYEE
1. Complete items one (1) through twenty-two (22) in full.
2. Complete items 23-27 only if other medical coverage exists.
3. Be certain to sign the authorization to release information block (28).
4. If you wish to have your benefits for this claim paid directly to your physician or supplier, sign the block (29).
5. If you have submitted a request for benefits to another plan, including Medicare, attach a copy of the bills you submitted
to the other plan and the explanation of benefits you received from the other plan.
6. Attach itemized bills or ask your health care provider to complete the applicable section on the reverse side. The bills
must include:
- patient's name
- date(s) of service(s)
- condition being treated
- relationship to employee
- type of service(s) rendered
If this information is missing, write it on the bill and sign your name.
7. If prescription drugs are covered under your plan, submit receipts or a Prescription Drug Record form. Receipt must
contain:
- drug name
- strength
- dose per/day
- prescription number
- charge
- quantity
- purchase date
- physician's name
- nature of illness or injury
- pharmacy name/address
This information can be copied from the prescription bottle or box.
8. Retain copies of your bills for your record.
9. Send the completed benefits request and the bills to the Aetna office address listed on the back of your medical
ID card.
TO THE PHYSICIAN OR SUPPLIER
1. Complete items thirty (30) through forty-eight (48) in full.
2. If the employee indicates that benefits should be paid directly to the physician or supplier, then these benefits will be sent
directly to you with an information copy of the transactions to the employee.
GC-7 (12-05)
R-POD
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1 2
2








