Quickcharts Patient Case History Template - Short Form Page 2
ADVERTISEMENT
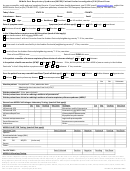
Date of last physical examination: _________________ Do you smoke
- how many per day? _________________
- how many per day? _________________
Do you exercise
__________________________________________________
PLEASE MARK YOUR AREAS OF PAIN ON THE DIAGRAM BELOW
Main reason for consulting the office:
Become pain free
Explanation of my condition
Learn how to care for my condition
Reduce symptoms
Resume normal activity level
What is your major complaint? _________________________________Date problem began? _____________________
How did this problem begin (falling, lifting, etc.)? _________________________________________________________
How is your condition changing?
GETTING BETTER
GETTING
NOT CHANGING
Have you had this condition in the past? YES - NO
How often do you experience your symptoms?
Constantly (76-100% of the day
Frequently (51-75% of the day)
Occasionally (26-50% of the day
Intermittently (0-25% of the day)
Describe the nature of your symptoms:
Sharp
Dull
Numb
Burning
Shooting
Tingling
Radiating Pain
Tightness
Stabbing
Throbbing
Other: __________________________________________________________
Please rate your pain on a scale of 1 to 10 (0= no pain and 10= excruciating pain)
1
2
3
4
5
6
7
8
9
10
How do your symptoms affect your ability to perform daily activities such as working or driving?
(0= no effect and 10= no possible activities)
1
2
3
4
5
6
7
8
9
10
What activities aggravate your condition (working, exercise, etc)? _____________________________________________
What makes your pain better (ice, heat, massage, etc)? ______________________________________________________
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2 3
3 4
4