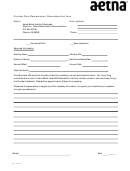
Please indicate the reason for resubmission and any pertinent details regarding your claim below.
Claim/Reconsideration Descriptions
Itemized Bill
•
All claims associated with an Itemized Bill must be broken out per Rev code to verify charges billed on the
UB match the charges billed on the Itemized bill. (Please attach I-Bill that is broken out by rev code with
sub-totals.)
Duplicate Claim
•
Review request for a claim whose original reason for denial was “duplicate.”
•
Provide documentation as to why the claim or service is not a duplicate such as medical records showing
two services were performed.
Corrected Claim
•
The corrected claim must be clearly identified as a corrected claim by writing or stamping “corrected” on
the claim itself.
Coordination of Benefits
•
Attach EOB or letter from primary carrier and forward to the claims department identifying as “corrected”
claim.
Proof of Timely Filing
•
For electronically submitted claims provide the second level acceptance report.
•
Refer to Proof of Timely Filing Requirements in your Provider Manual.
Claim/Coding Edit
•
Aetna Better Health of Missouri uses two (2) claims edit applications: Claim Check and iHealth. Please
refer to the Provider Manual on the Aetna Better Health of Missouri website
for more information on claim editing.
Corrected claims must be received within 180 days of the date on the first remittance advice. Please
refer to the Aetna Better Health of Missouri Provider Manual at ,
Claims and Reimbursement Procedures section for more information.
Appeals must be received within 180 days of the date of the incident causing the appeal. Please refer to
the Aetna Better Health of Missouri Provider Manual online at .
MO-15-04-78
Form code: PARF
Revised 7/29/2015
 1
1 2
2