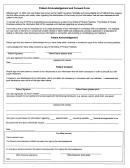
Patient History And Physical Form Page 2
ADVERTISEMENT
1. What is the reason for your visit today?_____________________________________________________________
Location: ______________________________________ Severity (1-10): ____________________________________
Duration: ______________________________________ Associated Symptoms: _______________________________
HEIGHT: _______________
WEIGHT: _______________ SHOE SIZE:_____________
Yes
No
2. Have you had the flu shot this season?
Yes
No
3. Are you or do you think you may be pregnant?
4. MEDICAL HISTORY-Please circle all that apply:
AIDS/HIV
Blood Disorder
Liver Disease
Tuberculosis or Exposure
Anemia
Cancer
Lung Disorder
Heart Conditions: ____________________________________
Arthritis
Congestive Heart
Seizure Disorder
Infectious Disease: ___________________________________
Failure
Asthma
Diabetes
Stroke
Stomach Problems: __________________________________
Blood Clots
High Blood Pressure
Thyroid Disorder
Other:________________________________________________
Sleep Apnea-If yes, do you use a CPAP? Yes No Setting: _______
5. SURGICAL HISTORY: Please list all surgeries ______________________________________________________
__________________________________________________________________________________________________
6. ALLERGY HISTORY: Do you have any allergies? (Medication or other): Yes
No
*IF YES, PLEASE LIST: __________________________________________________________________
_______________________________________________________________________________________
Have you had any complications with Anesthesia? No Yes__________________________________
7. MEDICATIONS: Please list any medications you are currently taking. Please include over-the-counter
medications. (If you have a medication list, we can make a copy).
8. FAMILY HISTORY-Please check all that apply:
Father
Mother
Brother
Sister
Son
Daughter
Anesthesia Complications
Bleeding Disorders
Blood clots
Cancer
Diabetes
Heart Attack or Angina
Heart Disease
High Blood Pressure
Stroke
Tuberculosis
9. SOCIAL HISTORY: Alcohol Use:
Smoking Use:
Illicit Drug Use:
Non-Drinker
Never Smoked
Never Used
Social Drinker
Current Smoker
Currently Using
Moderate Drinker
Former Smoker
Previously Used
Heavy Drinker
Recovering Drug Addict
Recovering Alcoholic
Patient/Guardian Signature _______________________________________________ Date: ____________________
If other than patient, please identify the relationship: ______________________________________________
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2