Us Standard Certificate Of Death Page 3
ADVERTISEMENT
Cause-of-death – Background, Examples, and Common Problems
Accurate cause of death information is important
•to the public health community in evaluating and improving the health of all citizens, and
•often to the family, now and in the future, and to the person settling the decedent’s estate.
The cause-of-death section consists of two parts. Part I is for reporting a chain of events leading directly to death, with the immediate cause of death (the final disease, injury, or complication directly causing death) on
line a and the underlying cause of death (the disease or injury that initiated the chain of events that led directly and inevitably to death) on the lowest used line. Part II is for reporting all other significant diseases,
conditions, or injuries that contributed to death but which did not result in the underlying cause of death given in Part I. The cause-of-death information should be YOUR best medical OPINION. A condition can be
listed as “probable” even if it has not been definitively diagnosed.
Examples of properly completed medical certifications
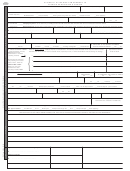
CAUSE OF DEATH (See instructions and examples)
Approximate interval:
Onset to death
32. PART I. Enter the chain of events--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
lines if necessary.
IMMEDIATE CAUSE (Final
Minutes
Rupture of myocardium
disease or condition --------->
a.
__________________________________________________________________________________
resulting in death)
Due to (or as a consequence of):
6 days
Acute myocardial infarction
Sequentially list conditions,
b.
_______________________________________________________________________________
if any, leading to the cause
Due to (or as a consequence of):
listed on line a. Enter the
5 years
Coronary artery thrombosis
UNDERLYING CAUSE
c.
_______________________________________________________________________________
(disease or injury that
Due to (or as a consequence of):
initiated the events resulting
7 years
Atherosclerotic coronary artery disease
in death) LAST
d.
__________________________________________________________________
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
■ Yes
No
Diabetes, Chronic obstructive pulmonary disease, smoking
34. WERE AUTOPSY FINDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? ■ Yes
No
35.
DID TOBACCO USE CONTRIBUTE TO DEATH?
36. IF FEMALE:
37. MANNER OF DEATH
■ Not pregnant within past year
■
■ Natural
Yes
Probably
Pregnant at time of death
Homicide
Not pregnant, but pregnant within 42 days of death
Accident
Pending Investigation
No
Unknown
Suicide
Could not be determined
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
Approximate interval:
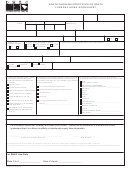
CAUSE OF DEATH (See instructions and examples)
Onset to death
32. PART I. Enter the chain of events--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
lines if necessary.
IMMEDIATE CAUSE (Final
2 Days
Aspiration pneumonia_______________________________________________________________
disease or condition --------->
a.
resulting in death)
Due to (or as a consequence of):
7 weeks
Complications of coma
Sequentially list conditions,
b.
___________________________________________________________________________________
if any, leading to the cause
Due to (or as a consequence of):
listed on line a. Enter the
7 weeks
Blunt force injuries
UNDERLYING CAUSE
c.
________________________________________________________________________________________
(disease or injury that
Due to (or as a consequence of):
initiated the events resulting
Motor vehicle accident
in death) LAST
d.
____________________________________________________________________________________
7 weeks
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
■ Yes
No
34. WERE AUTOPSY FINDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? ■ Yes
No
35.
DID TOBACCO USE CONTRIBUTE TO DEATH?
36. IF FEMALE:
37. MANNER OF DEATH
Not pregnant within past year
Yes
Probably
Natural
Homicide
Pregnant at time of death
■ Accident
Pending Investigation
Not pregnant, but pregnant within 42 days of death
■ No
Unknown
Suicide
Could not be determined
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
38. DATE OF INJURY
39. TIME OF INJURY
40. PLACE OF INJURY (e.g., Decedent’s home; construction site; restaurant; wooded area)
41. INJURY AT WORK?
(Mo/Day/Yr) (Spell Month)
Approx. 2320
road side near state highway
Yes ■ No
August 15, 2003
42. LOCATION OF INJURY:
State: Missouri
City or Town: near Alexandria
Street & Number: mile marker 17 on state route 46a
Apartment No.:
Zip Code:
43. DESCRIBE HOW INJURY OCCURRED:
44. IF TRANSPORTATION INJURY, SPECIFY:
■ Driver/Operator
Decedent driver of van, ran off road into tree
Passenger
Pedestrian
Other (Specify)
Common problems in death certification
The elderly decedent should have a clear and distinct etiological sequence for cause of death, if possible. Terms such as senescence, infirmity, old age, and advanced age have little value for public health or medical
research. Age is recorded elsewhere on the certificate. When a number of conditions resulted in death, the physician should choose the single sequence that, in his or her opinion, best describes the process leading to
death, and place any other pertinent conditions in Part II. If after careful consideration the physician cannot determine a sequence that ends in death, then the medical examiner or coroner should be consulted about
conducting an investigation or providing assistance in completing the cause of death.
The infant decedent should have a clear and distinct etiological sequence for cause of death, if possible. “Prematurity” should not be entered without explaining the etiology of prematurity. Maternal conditions may have
initiated or affected the sequence that resulted in infant death, and such maternal causes should be reported in addition to the infant causes on the infant’s death certificate (e.g., Hyaline membrane disease due to
prematurity, 28 weeks due to placental abruption due to blunt trauma to mother’s abdomen).
When SIDS is suspected, a complete investigation should be conducted, typically by a medical examiner or coroner. If the infant is under 1 year of age, no cause of death is determined after scene investigation, clinical
history is reviewed, and a complete autopsy is performed, then the death can be reported as Sudden Infant Death Syndrome.
When processes such as the following are reported, additional information about the etiology should be reported:
Abscess
Carcinomatosis
Disseminated intra vascular
Hyponatremia
Pulmonary arrest
Abdominal hemorrhage
Cardiac arrest
coagulopathy
Hypotension
Pulmonary edema
Adhesions
Cardiac dysrhythmia
Dysrhythmia
Immunosuppression
Pulmonary embolism
Adult respiratory distress syndrome
Cardiomyopathy
End-stage liver disease
Increased intra cranial pressure
Pulmonary insufficiency
Acute myocardial infarction
Cardiopulmonary arrest
End-stage renal disease
Intra cranial hemorrhage
Renal failure
Altered mental status
Cellulitis
Epidural hematoma
Malnutrition
Respiratory arrest
Anemia
Cerebral edema
Exsanguination
Metabolic encephalopathy
Seizures
Anoxia
Cerebrovascular accident
Failure to thrive
Multi-organ failure
Sepsis
Anoxic encephalopathy
Cerebellar tonsillar herniation
Fracture
Multi-system organ failure
Septic shock
Arrhythmia
Chronic bedridden state
Gangrene
Myocardial infarction
Shock
Ascites
Cirrhosis
Gastrointestinal hemorrhage
Necrotizing soft-tissue infection
Starvation
Aspiration
Coagulopathy
Heart failure
Old age
Subdural hematoma
Atrial fibrillation
Compression fracture
Hemothorax
Open (or closed) head injury
Subarachnoid hemorrhage
Bacteremia
Congestive heart failure
Hepatic failure
Paralysis
Sudden death
Bedridden
Convulsions
Hepatitis
Pancytopenia
Thrombocytopenia
Biliary obstruction
Decubiti
Hepatorenal syndrome
Perforated gallbladder
Uncal herniation
Bowel obstruction
Dehydration
Hyperglycemia
Peritonitis
Urinary tract infection
Brain injury
Dementia (when not
Hyperkalemia
Pleural effusions
Ventricular fibrillation
Brain stem hern tion
ia
otherw e specified)
is
Hypovolemic shock
Pneumonia
Ventricular tachyc rdia
a
Carcinogenesis
Diarrhea
Volume depletion
If the certifier is unable to determine the etiology of a process such as those shown above, the process must be qualified as being of an unknown, undetermined, probable, presumed, or unspecified etiology so it is clear
that a distinct etiology was not inadvertently or carelessly omitted.
The following conditions and types of death might seem to be specific or natural but when the medical history is examined further may be found to be complications of an injury or poisoning (possibly occurring long ago).
Such cases should be reported to the medical examiner/coroner.
Asphyxia
Epidural hematoma
Hip fracture
Pulmonary emboli
Subdural hematoma
Bolus
Exsanguination
Hyperthermia
Seizure disorder
Surgery
Choking
Fall
Hypothermia
Sepsis
Thermal burns/chemical burns
Drug or alcohol verdose/drug or
o
Fracture
Open reduction of fracture
Subarachnoid hemorrhage
alcohol abuse
REV. 11/2003
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1 2
2 3
3 4
4