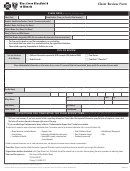
2013 Enrollment Application/change Form - Blue Cross And Blueshield Of Texas Page 2
ADVERTISEMENT
ENROLLMENT APPLICATION / CHANGE FORM INSTRUCTIONS
PLEASE READ THOROUGHLY BEFORE COMPLETING ENROLLMENT APPLICATION / CHANGE FORM
Use a black or blue ballpoint pen only. Print neatly. Do not abbreviate.
Please Note: If your group offers a Consumer Choice health plan you have the option to choose a Consumer Choice
of Benefits Health Insurance Plan or Consumer Choice of Benefits Health Maintenance Organization health care plan
that, either in whole or in part, does not provide state-mandated health benefits normally required in accident and
sickness insurance policies or evidences of coverage in Texas. This standard health benefit plan may provide a more
affordable health insurance policy or health plan for you, although, at the same time, it may provide you with fewer
health benefits than those normally included as state-mandated health benefits in policies or evidences of coverage in
Texas. If you choose this standard health benefit plan, please consult with your insurance agent to discover which
state-mandated health benefits are excluded in this policy or evidence of coverage (Certificate of Coverage).
SECTION 1
Check all the boxes that apply to indicate if you are a new enrollee or if you are requesting a change to your coverage. Indicate the event and date, if applicable. Complete the
additional sections that correspond to your selection.
New Enrollee: Complete all Sections where applicable.
dd Dependent: Complete all Sections where applicable.
• If you are adding or enrolling a dependent due to court order, you must submit a copy of the court order or decree AND a completed Dependent Addition and Change
Form for Court-Mandated Health Coverage.
• If student dependent coverage is part of your employer’s plan and you are adding or enrolling a dependent child age 26 or over who is a student, you may be required
to submit a completed Student Certification form.
• If you are applying for coverage for a disabled dependent child over the dependent age limit of your employer’s plan, you are required to submit a completed Dependent
Child’s Statement of Disability form. A disabled dependent over the dependent age limit of your employer’s plan must be certified by medical underwriting.
Cancel Enrollee: Complete Sections 1, 2, 4, and 11. In Section 4 include name, social security number, and date of birth of individual(s) cancelling.
Cancel Dependent: Complete Sections 1, 2, 4, and 11. In Section 4 include name and date of birth of individual(s) cancelling.
Declining Coverage: Complete Sections 2, 10, and 11.
SECTIONS 2 & 3
Complete all areas that apply to you.
Complete all areas that apply to you and each dependent.
SECTION 4
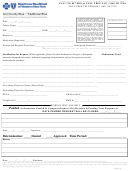
For HMO and POS only: Those applying for HMO or POS coverage should select a PCP for each individual to be covered. List the name of the physician and the provider number
from the provider directory or Provider Finder at www. c . Be sure to check the appropriate box for a new patient.
TTENTION FEM LE MEMBERS: In selecting your PCP, remember that your PCP’s network may affect your choice of an OB/GYN. You have the right to receive services from an
OB/GYN without first obtaining a referral from your PCP. However, for HMO members, the OB/GYN from whom you receive services must belong to the same physician practice
group or independent practice association (IPA) as your PCP. This is another reason to make certain that your PCP's network includes the specialists – particularly the OB/GYN –
and hospitals that you prefer. You are not required to designate an OB/GYN. You may elect to receive OB/GYN services from your PCP.
Change Primary Care Physician (PCP): In Section 1, check the “Other Change(s)” box, then complete sections 2, 3, 4, and 11. In Section 4, please include enrollee's or
dependent’s name, social security number, date of birth, and name and number of the new PCP.
Change ddress / Name: In Section 1, check the “Other Change(s)” box, then complete sections 1, 2, and 11.
Complete this section if your employer is offering life insurance coverage.
SECTION 5
SECTION 6
Complete this section if you are applying for coverage for a disabled dependent child over the dependent child age limit of your employer’s plan. A disabled dependent must be
certified by medical underwriting and a completed Dependent Child’s Statement of Disability form must be submitted with this enrollment application.
SECTION 7
Complete this section unless you are applying for HMO or In-Hospital Indemnity coverage.
The health coverage for which you are applying may have a preexisting condition waiting period. On your group's first contract date or contract anniversary date on or after
September 23, 2010, a preexisting condition waiting period will not apply for individuals under the age of 19. Check with your employer if you have questions regarding
preexisting condition waiting period applicability for individuals under the age of 19.
Complete this section if you or any dependent have other health care coverage through an employer (group coverage) that will not be cancelled when the coverage under this
SECTION 8
application becomes effective.
Complete this section if you or any of your dependents are covered by Medicare.
SECTION 9
SECTION 10
Complete this section if you are declining health coverage for yourself and your dependents. nyone declining coverage for any reason should complete Section 10, not just
those declining because of other coverage.
IMPORT NT NOTICE – DECLIN TION OF HE LTH COVER GE
If you are declining enrollment for yourself or your dependents (including your spouse) because of other health care coverage, you may, in
the future, be able to enroll yourself or your dependents in the plan if you request enrollment within 31 days after your other coverage ends.
In addition, if you have a new dependent as a result of a marriage, birth, adoption or becoming a party in a suit for adoption, you may be
able to enroll yourself and your dependents if you request enrollment within 31 days after the marriage, birth, adoption or suit for adoption.
Sign your name and date the enrollment application if you agree to the conditions set forth in this section. Your enrollment application should be submitted to your employer’s
SECTION 11
Enrollment Department, which will then submit your form to: Group ccounts Dept. • P. O. Box 655730 • Dallas, TX 75265-5730
Changes in state or federal law or regulations, or interpretations thereof, may change the terms and conditions of coverage.
Forms referenced above may be obtained by accessing the BCBSTX website at www. c , from your Marketing Service
Representative, or from your employer. If you have any questions, please contact your Marketing Service Representative.
54521.1012
EA/CF 1012
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1 2
2 3
3 4
4