Uniform Treatment Plan Form Page 3
ADVERTISEMENT
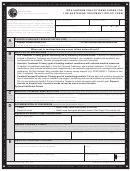
Primary reason for request or admission: (check one)
Self/Other Lethality Issues
Violent, unpredictable/uncontrolled behavior
Safety issues
Eating Disorder
Detox/withdrawal symptoms
Substance Use
Psychosis
Mania
Depression
Other ________________________________________
Why does this patient require this higher level of care at this time? (Please provide frequency, intensity , duration of impairing behaviors and
symptoms):______________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
Medication adjustments (medication name and dose) during level of care: __________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
Barriers to Compliance or Adherence: _______________________________________________________________________________________
Prior Treatment in past 6 months:
Mental Health
Substance Use Disorder
Inpatient
Residential
Partial
Intensive Outpatient
Outpatient
Relevant Medical issues (if any): _____________________________________________________________________________________________
________________________________________________________________________________________________________________________
Support System/Home Environment: _________________________________________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
Treatment Plan (include objectives, goals and interventions):_______________________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
If Concurrent Review—What progress has been made since the last review___________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
Why does member continue to need level of care________________________________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
Discharge Plan (including anticipated discharge date)_____________________________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
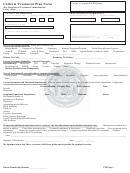
Complete the following if substance use is present for higher level of care requests:
Type of substance use disorder ________________________________________________
Onset:
Recent
Past 12 Months
More than 12 months ago
Frequency:
Daily
Few Times Per Week
Few Times Per Month
Binge Pattern
Last Used:
Past Week
Past Month
Past 3 Months
Past Year
More than one year ago
Consequences of relapse:
Medical
Social
Housing
Work/School
Legal
Other __________________________________________
Urine Drug Screen:
Yes
No
Vital Signs: ____________________________________________________________________________
Current Withdrawal Score: (CIWA____________ COWS_____________) or Symptoms (
check if not applicable) _________________________
________________________________________________________________________________________________________________________
History of:
Seizures
DT’s
Blackouts
Other
Not Applicable
Complete the following if the request is related to the treatment of an eating disorder for higher level of care requests:
Height: _____ Weight:_______ % of NBW_________
Highest weight___________ Lowest weight______________ Weight change over time (e.g. lbs lost in 1 month) ______________
If purging, type and frequency ____________ Potassium _________ Sodium _________ Vital signs ___________
Abnormal EKG____________
Medical Evaluation
Yes
No
Please identify current symptoms, behaviors and diagnosis of any Eating Disorder issues: _______________________________________________
________________________________________________________________________________________________________________________
Please include any current medical/physiological pathologic manifestations: __________________________________________________________
________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2 3
3