Form Lhl009/0116 Request For A Review By An Independent Review Organization (Iro) - Texas Department Of Insurance
ADVERTISEMENT
LHL009/0116
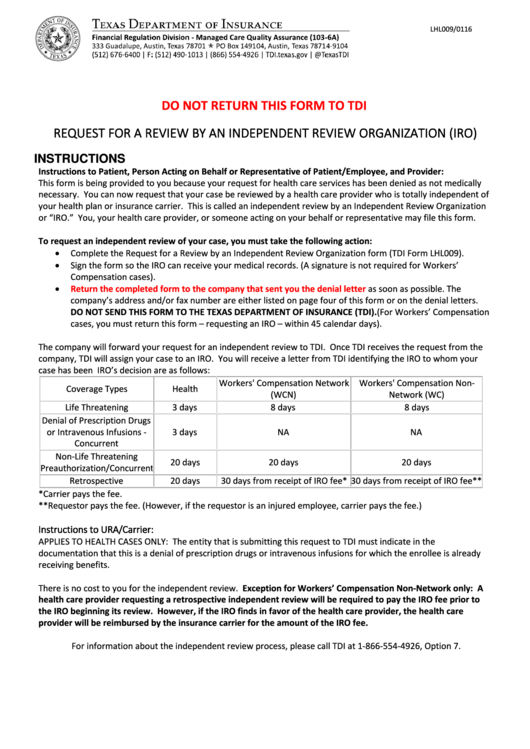
DO NOT RETURN THIS FORM TO TDI
REQUEST FOR A REVIEW BY AN INDEPENDENT REVIEW ORGANIZATION (IRO)
INSTRUCTIONS
Instructions to Patient, Person Acting on Behalf or Representative of Patient/Employee, and Provider:
This form is being provided to you because your request for health care services has been denied as not medically
necessary. You can now request that your case be reviewed by a health care provider who is totally independent of
your health plan or insurance carrier. This is called an independent review by an Independent Review Organization
or “IRO.” You, your health care provider, or someone acting on your behalf or representative may file this form.
To request an independent review of your case, you must take the following action:
Complete the Request for a Review by an Independent Review Organization form (TDI Form LHL009).
Sign the form so the IRO can receive your medical records. (A signature is not required for Workers’
Compensation cases).
Return the completed form to the company that sent you the denial letter
as soon as possible. The
company’s address and/or fax number are either listed on page four of this form or on the denial letters.
DO NOT SEND THIS FORM TO THE TEXAS DEPARTMENT OF INSURANCE (TDI). (For Workers’ Compensation
cases, you must return this form – requesting an IRO – within 45 calendar days).
The company will forward your request for an independent review to TDI. Once TDI receives the request from the
company, TDI will assign your case to an IRO. You will receive a letter from TDI identifying the IRO to whom your
case has been assigned. The timeframes for an IRO’s decision are as follows:
Workers' Compensation Network
Workers' Compensation Non-
Coverage Types
Health
(WCN)
Network (WC)
Life Threatening
3 days
8 days
8 days
Denial of Prescription Drugs
or Intravenous Infusions -
3 days
NA
NA
Concurrent
Non-Life Threatening
20 days
20 days
20 days
Preauthorization/Concurrent
Retrospective
20 days
30 days from receipt of IRO fee* 30 days from receipt of IRO fee**
*Carrier pays the fee.
**Requestor pays the fee. (However, if the requestor is an injured employee, carrier pays the fee.)
Instructions to URA/Carrier:
APPLIES TO HEALTH CASES ONLY: The entity that is submitting this request to TDI must indicate in the
documentation that this is a denial of prescription drugs or intravenous infusions for which the enrollee is already
receiving benefits.
There is no cost to you for the independent review. Exception for Workers’ Compensation Non-Network only: A
health care provider requesting a retrospective independent review will be required to pay the IRO fee prior to
the IRO beginning its review. However, if the IRO finds in favor of the health care provider, the health care
provider will be reimbursed by the insurance carrier for the amount of the IRO fee.
For information about the independent review process, please call TDI at 1-866-554-4926, Option 7.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1 2
2 3
3 4
4