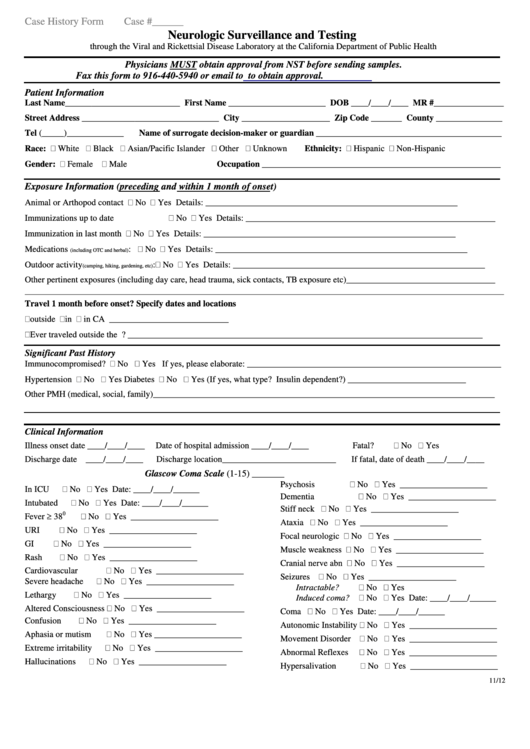
Case History Form - Neurologic Surveillance Testing
ADVERTISEMENT
Case History Form
Case #______
Neurologic Surveillance and Testing
through the Viral and Rickettsial Disease Laboratory at the California Department of Public Health
Physicians MUST obtain approval from NST before sending samples.
Fax this form to 916-440-5940 or email to
NeuroSurveillance@cdph.ca.gov
to obtain approval.
Patient Information
Last Name__________________________ First Name ______________________ DOB ____/____/____ MR #________________
Street Address _______________________________ City ____________________ Zip Code _______ County _______________
Tel (_____)_____________
Name of surrogate decision-maker or guardian __________________________________________
Race:
White
Black
Asian/Pacific Islander
Other
Unknown
Ethnicity:
Hispanic
Non-Hispanic
Gender:
Female
Male
Occupation ______________________________________________________
Exposure Information (preceding and within 1 month of onset)
Animal or Arthopod contact
No
Yes Details: _________________________________________________________
Immunizations up to date
No
Yes Details: _________________________________________________________
Immunization in last month
No
Yes Details: _________________________________________________________
Medications
:
No
Yes Details: _________________________________________________________
(including OTC and herbal)
Outdoor activity
:
No
Yes Details: _________________________________________________________
(camping, hiking, gardening, etc)
Other pertinent exposures (including day care, head trauma, sick contacts, TB exposure etc)__________________________________
___________________________________________________________________________________________________________________________________________________________________________________
Travel 1 month before onset? Specify dates and locations
outside U.S. __________________________
in U.S. _________________________
in CA ___________________________
Ever traveled outside the U.S.? _________________________________________________________________________________
Significant Past History
Immunocompromised?
No
Yes If yes, please elaborate: __________________________________________________________
Hypertension
No
Yes
Diabetes
No
Yes (If yes, what type? Insulin dependent?) ___________________________
Other PMH (medical, social, family)______________________________________________________________________________
Clinical Information
Illness onset date ____/____/____
Date of hospital admission ____/____/____
Fatal?
No
Yes
Discharge date ____/____/____
Discharge location__________________________
If fatal, date of death ____/____/____
Glascow Coma Scale (1-15) _______
Psychosis
No
Yes ____________________
In ICU
No
Yes Date: ____/____/______
Dementia
No
Yes ____________________
Intubated
No
Yes Date: ____/____/______
Stiff neck
No
Yes ____________________
Fever 38
0
No
Yes ____________________
Ataxia
No
Yes ____________________
URI
No
Yes ____________________
Focal neurologic
No
Yes ____________________
GI
No
Yes ____________________
Muscle weakness
No
Yes ____________________
Rash
No
Yes ____________________
Cranial nerve abn
No
Yes ____________________
Cardiovascular
No
Yes ____________________
Seizures
No
Yes ____________________
Severe headache
No
Yes ____________________
Intractable?
No
Yes
Lethargy
No
Yes ____________________
Induced coma?
No
Yes Date: ____/____/______
Altered Consciousness
No
Yes ____________________
Coma
No
Yes Date: ____/____/______
Confusion
No
Yes ____________________
Autonomic Instability
No
Yes ____________________
Aphasia or mutism
No
Yes ____________________
Movement Disorder
No
Yes ____________________
Extreme irritability
No
Yes ____________________
Abnormal Reflexes
No
Yes ____________________
Hallucinations
No
Yes ____________________
Hypersalivation
No
Yes ____________________
11/12
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2








