Ampyra (Dalfampridine Er) Prior Authorization Of Benefits (Pab) Form
ADVERTISEMENT
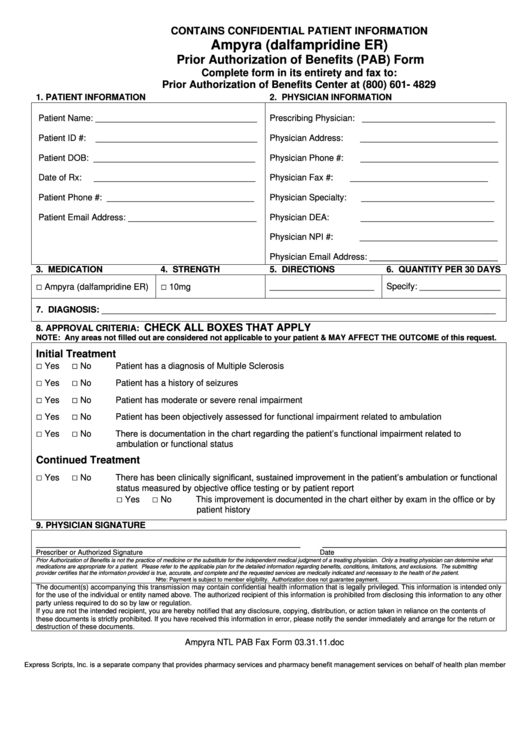
CONTAINS CONFIDENTIAL PATIENT INFORMATION
Ampyra (dalfampridine ER)
Prior Authorization of Benefits (PAB) Form
Complete form in its entirety and fax to:
Prior Authorization of Benefits Center at (800) 601- 4829
1. PATIENT INFORMATION
2. PHYSICIAN INFORMATION
Patient Name: __________________________________
Prescribing Physician: ____________________________
Patient ID #:
__________________________________
Physician Address:
_____________________________
Patient DOB: __________________________________
Physician Phone #:
_____________________________
Date of Rx:
__________________________________
Physician Fax #:
_____________________________
Patient Phone #: _______________________________
Physician Specialty:
____________________________
Patient Email Address: ___________________________
Physician DEA:
____________________________
Physician NPI #:
_____________________________
Physician Email Address: ___________________________
3. MEDICATION
4. STRENGTH
5. DIRECTIONS
6. QUANTITY PER 30 DAYS
□
□
______________________
Specify: _________________
Ampyra (dalfampridine ER)
10mg
7. DIAGNOSIS: ___________________________________________________________________________________
CHECK ALL BOXES THAT APPLY
8. APPROVAL CRITERIA:
NOTE: Any areas not filled out are considered not applicable to your patient & MAY AFFECT THE OUTCOME of this request.
Initial Treatment
□
□
Yes
No
Patient has a diagnosis of Multiple Sclerosis
□
□
Yes
No
Patient has a history of seizures
□
□
Yes
No
Patient has moderate or severe renal impairment
□
□
Yes
No
Patient has been objectively assessed for functional impairment related to ambulation
□
□
There is documentation in the chart regarding the patient’s functional impairment related to
Yes
No
ambulation or functional status
Continued Treatment
□
□
There has been clinically significant, sustained improvement in the patient’s ambulation or functional
Yes
No
status measured by objective office testing or by patient report
□
□
Yes
No
This improvement is documented in the chart either by exam in the office or by
patient history
9. PHYSICIAN SIGNATURE
____________________________________________________________
__________________________________________
Prescriber or Authorized Signature
Date
Prior Authorization of Benefits is not the practice of medicine or the substitute for the independent medical judgment of a treating physician. Only a treating physician can determine what
medications are appropriate for a patient. Please refer to the applicable plan for the detailed information regarding benefits, conditions, limitations, and exclusions. The submitting
provider certifies that the information provided is true, accurate, and complete and the requested services are medically indicated and necessary to the health of the patient.
Note: Payment is subject to member eligibility. Authorization does not guarantee payment.
The document(s) accompanying this transmission may contain confidential health information that is legally privileged. This information is intended only
for the use of the individual or entity named above. The authorized recipient of this information is prohibited from disclosing this information to any other
party unless required to do so by law or regulation.
If you are not the intended recipient, you are hereby notified that any disclosure, copying, distribution, or action taken in reliance on the contents of
these documents is strictly prohibited. If you have received this information in error, please notify the sender immediately and arrange for the return or
destruction of these documents.
Ampyra NTL PAB Fax Form 03.31.11.doc
Express Scripts, Inc. is a separate company that provides pharmacy services and pharmacy benefit management services on behalf of health plan members.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1








