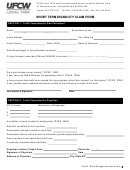
Short Term Disability Claim Form Initial Assessment Page 2
ADVERTISEMENT
Part 2 - ATTENDING PHYSICIAN’S STATEMENT – INITIAL ASSESSMENT
Authorization/Consent
I authorize any licensed physician, medical practitioner or health care professional who has observed me for diagnosis or treatment, any hospital,
clinic, or other medical or medically related facility where I have been a patient, any public body,
private health or social establishment, personal information agency, market intermediary, insurance company, institution, current or former
employer, or person, to release to Coughlin & Associates Ltd. or its agents the documentation they require to administer this claim. I authorize
Coughlin & Associates Ltd. to release such documentation to independent medical examiners, to my Plan Sponsor/Employer and to any other
insurance company, organization, establishment or body when Coughlin & Associates Ltd. deems it necessary for the purpose of administering
this claim. A photostat of this authorization is as valid as the original.
Patient Signature ______________________________
Patient Name _______________________________
____________________
Day
Month
Year
Note: The patient is responsible for obtaining this form and any charges for its completion, unless prohibited by law.
SECTION A: DIAGNOSIS
What is the primary diagnosis? _________________________________________________________________________________________
When did symptoms first appear or date accident occurred?
____________________
Day
Month
Year
What was the date of the patient’s first visit for his/her condition?
____________________
Day
Month
Year
Please indicate all dates of visits for the current condition:
Mth.
Year
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
Planned frequency of visits:
Weekly
Monthly
Other, specify: _____________________________________
Has the patient ever had the same or similar condition?
Yes
No
If yes, please elaborate: ___________________________
___________________________________________________________________________________________________________________
Is the patient’s condition due to injury or sickness arising out of his/her employment?
Yes
No
Is there a secondary diagnosis or additional complication which might affect the duration of absence from work?
Yes
No
If yes, please elaborate: _______________________________________________________________________________________________
Please list the patient’s symptoms (including severity and frequency) identifying which of the symptoms listed you have objectively observed:
___________________________________________________________________________________________________________________
___________________________________________________________________________________________________________________
What are the patient’s current limitations? Please be specific. _________________________________________________________________
___________________________________________________________________________________________________________________
What are the patient’s current restrictions? Please be specific. _______________________________________________________________
___________________________________________________________________________________________________________________
Please indicate the date the patient stopped working based on your recommendation.
____________________
Day
Month
Year
To the best of my knowledge, the patient has been totally disabled,
From _____________________
To ______________________
Day
Month
Year
Day
Month
Year
Please provide date when patient should be able to return to work. _____________________
Day
Month
Year
SECTION B: TREATMENT
Has the patient been hospitalized?
Yes
No
If yes, please provide the name of the hospital and the date(s) of confinement. ___________________________________________________
If surgery was performed, please provide a description and date(s). _____________________________________________________________
Please detail the patient’s past and present treatment as well as response to treatment. _____________________________________________
___________________________________________________________________________________________________________________
Please list all medications that the patient is currently taking, including dosage and date prescribed.
Medication
Dosage
Date Prescribed (D/M/Y)
If you have referred the patient to a specialist, please provide the name of the specialist(s) and area of specialty. _________________________
___________________________________________________________________________________________________________________
________________________________________
______________________________________________________________
Name (please print)
Address
Telephone No.
_____________
________________________________________
____________________________________
Date
Signature
Specialty
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1 2
2