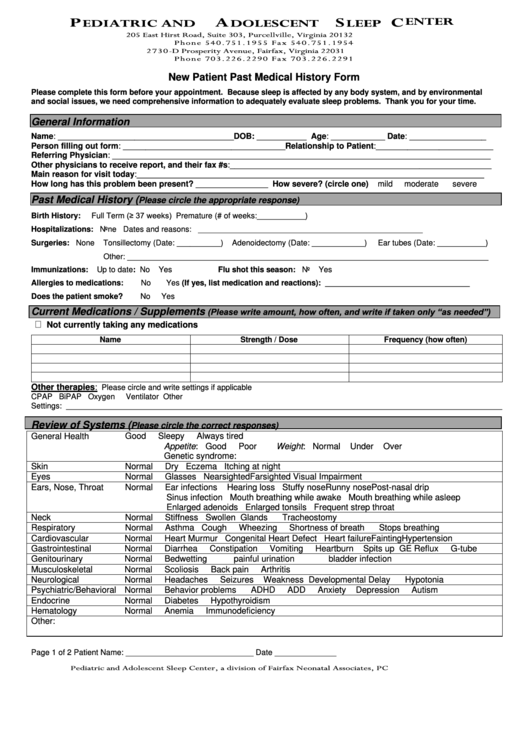
New Patient Past Medical History Form
ADVERTISEMENT
P
A
S
C
E D I A T R I C A N D
D O L E S C E N T
L E E P
E N T E R
2 0 5 E a s t H i r s t R o a d , S u i t e 3 0 3 , P u r c e l l v i l l e , V i r g i n i a 2 0 1 3 2
P h o n e 5 4 0 . 7 5 1 . 1 9 5 5 F a x 5 4 0 . 7 5 1 . 1 9 5 4
2 7 3 0 - D P r o s p e r i t y A v e n u e , F a i r f a x , V i r g i n i a 2 2 0 3 1
P h o n e 7 0 3 . 2 2 6 . 2 2 9 0 F a x 7 0 3 . 2 2 6 . 2 2 9 1
New Patient Past Medical History Form
Please complete this form before your appointment. Because sleep is affected by any body system, and by environmental
and social issues, we need comprehensive information to adequately evaluate sleep problems. Thank you for your time.
General Information
Name: _______________________________________ DOB: ___________ Age: ____________ Date: _________________
Person filling out form: ____________________________________Relationship to Patient:__________________________
Referring Physician: ____________________________________________________________________________________
Other physicians to receive report, and their fax #s:__________________________________________________________
Main reason for visit today:_____________________________________________________________________________
How long has this problem been present? ________________ How severe? (circle one)
mild
moderate
severe
Past Medical History (
Please circle the appropriate response)
Full Term (≥ 37 weeks)
Birth History:
Premature (# of weeks:___________)
Hospitalizations: None
Dates and reasons: ___________________________________________________
Surgeries: None
Tonsillectomy (Date: __________)
Adenoidectomy (Date: ____________)
Ear tubes (Date: ___________)
Other: __________________________________________________________________________________
Immunizations:
Up to date: No
Yes
Flu shot this season: No
Yes
Allergies to medications:
No
Yes
(If yes, list medication and reactions): _________________________________
Does the patient smoke?
No
Yes
(Please write amount, how often, and write if taken only “as needed”)
Current Medications / Supplements
Not currently taking any medications
Name
Strength / Dose
Frequency (how often)
Other therapies:
Please circle and write settings if applicable
CPAP
BiPAP
Oxygen
Ventilator
Other
Settings: ___________________________________________________________________________________________________
Review of Systems (
Please circle the correct responses)
General Health
Good
Sleepy
Always tired
Appetite: Good
Poor
Weight: Normal
Under
Over
Genetic syndrome:
Skin
Normal
Dry Eczema Itching at night
Eyes
Normal
Glasses Nearsighted Farsighted
Visual Impairment
Ears, Nose, Throat
Normal
Ear infections
Hearing loss Stuffy nose Runny nose Post-nasal drip
Sinus infection Mouth breathing while awake Mouth breathing while asleep
Enlarged adenoids Enlarged tonsils Frequent strep throat
Neck
Normal
Stiffness
Swollen Glands
Tracheostomy
Respiratory
Normal
Asthma Cough
Wheezing
Shortness of breath
Stops breathing
Cardiovascular
Normal
Heart Murmur Congenital Heart Defect Heart failure Fainting Hypertension
Gastrointestinal
Normal
Diarrhea
Constipation
Vomiting
Heartburn
Spits up GE Reflux
G-tube
Genitourinary
Normal
Bedwetting
painful urination
bladder infection
Musculoskeletal
Normal
Scoliosis
Back pain
Arthritis
Neurological
Normal
Headaches
Seizures
Weakness Developmental Delay
Hypotonia
Psychiatric/Behavioral Normal
Behavior problems
ADHD
ADD
Anxiety
Depression
Autism
Endocrine
Normal
Diabetes
Hypothyroidism
Hematology
Normal
Anemia
Immunodeficiency
Other:
Page 1 of 2
Patient Name: _____________________________ Date ______________
P e d i a t r i c a n d A d o l e s c e n t S l e e p C e n t e r , a d i v i s i o n o f F a i r f a x N e o n a t a l A s s o c i a t e s , P C
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2