Nih Stroke Scale
ADVERTISEMENT
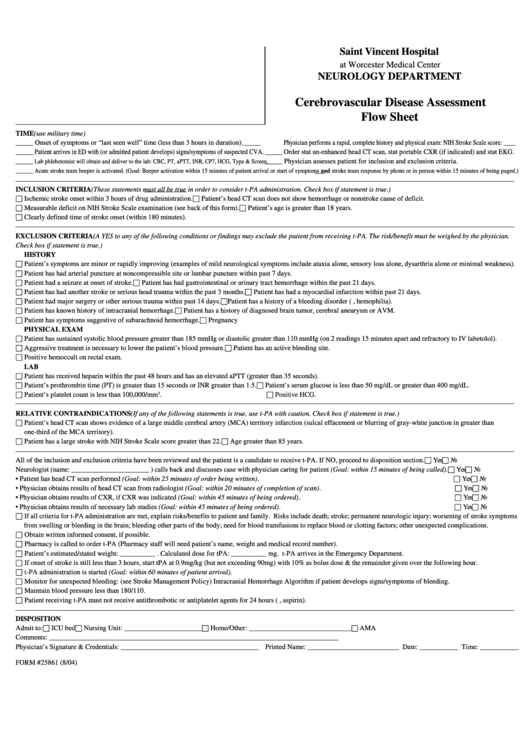
Saint Vincent Hospital
at Worcester Medical Center
NEUROLOGY DEPARTMENT
Cerebrovascular Disease Assessment
Flow Sheet
TIME (use military time)
_____ Onset of symptoms or “last seen well” time (less than 3 hours in duration).
_____ Physician performs a rapid, complete history and physical exam: NIH Stroke Scale score: ____
_____ Patient arrives in ED with (or admitted patient develops) signs/symptoms of suspected CVA. _____ Order stat un-enhanced head CT scan, stat portable CXR (if indicated) and stat EKG.
_____
_____ Physician assesses patient for inclusion and exclusion criteria.
Lab phlebotomist will obtain and deliver to the lab: CBC, PT, aPTT, INR, CP7, HCG, Type & Screen.
_____
Acute stroke team beeper is activated. (Goal: Beeper activation within 15 minutes of patient arrival or start of symptoms and stroke team response by phone or in person within 15 minutes of being paged.)
INCLUSION CRITERIA (These statements must all be true in order to consider t-PA administration. Check box if statement is true.)
□ Ischemic stroke onset within 3 hours of drug administration.
□ Patient’s head CT scan does not show hemorrhage or nonstroke cause of deficit.
□ Measurable deficit on NIH Stroke Scale examination (see back of this form).
□ Patient’s age is greater than 18 years.
□ Clearly defined time of stroke onset (within 180 minutes).
EXCLUSION CRITERIA (A YES to any of the following conditions or findings may exclude the patient from receiving t-PA. The risk/benefit must be weighed by the physician.
Check box if statement is true.)
HISTORY
□ Patient’s symptoms are minor or rapidly improving (examples of mild neurological symptoms include ataxia alone, sensory loss alone, dysarthria alone or minimal weakness).
□ Patient has had arterial puncture at noncompressible site or lumbar puncture within past 7 days.
□ Patient had a seizure at onset of stroke.
□ Patient has had gastrointestinal or urinary tract hemorrhage within the past 21 days.
□ Patient has had another stroke or serious head trauma within the past 3 months.
□ Patient has had a myocardial infarction within past 21 days.
□ Patient had major surgery or other serious trauma within past 14 days.
□ Patient has a history of a bleeding disorder (e.g., hemophilia).
□ Patient has known history of intracranial hemorrhage.
□ Patient has a history of diagnosed brain tumor, cerebral aneurysm or AVM.
□ Patient has symptoms suggestive of subarachnoid hemorrhage.
□ Pregnancy
PHYSICAL EXAM
□ Patient has sustained systolic blood pressure greater than 185 mmHg or diastolic greater than 110 mmHg (on 2 readings 15 minutes apart and refractory to IV labetolol).
□ Aggressive treatment is necessary to lower the patient’s blood pressure.
□ Patient has an active bleeding site.
□ Positive hemoccult on rectal exam.
LAB
□ Patient has received heparin within the past 48 hours and has an elevated aPTT (greater than 35 seconds).
□ Patient’s prothrombin time (PT) is greater than 15 seconds or INR greater than 1.5.
□ Patient’s serum glucose is less than 50 mg/dL or greater than 400 mg/dL.
□ Patient’s platelet count is less than 100,000/mm
□ Positive HCG.
3
.
RELATIVE CONTRAINDICATIONS (If any of the following statements is true, use t-PA with caution. Check box if statement is true.)
□ Patient’s head CT scan shows evidence of a large middle cerebral artery (MCA) territory infarction (sulcal effacement or blurring of gray-white junction in greater than
one-third of the MCA territory).
□ Patient has a large stroke with NIH Stroke Scale score greater than 22.
□ Age greater than 85 years.
□ Yes
□ No
All of the inclusion and exclusion criteria have been reviewed and the patient is a candidate to receive t-PA. If NO, proceed to disposition section.
□ Yes
□ No
Neurologist (name: ______________________ ) calls back and discusses case with physician caring for patient (Goal: within 15 minutes of being called).
□ Yes
□ No
• Patient has head CT scan performed (Goal: within 25 minutes of order being written).
□ Yes
□ No
• Physician obtains results of head CT scan from radiologist (Goal: within 20 minutes of completion of scan).
□ Yes
□ No
• Physician obtains results of CXR, if CXR was indicated (Goal: within 45 minutes of being ordered).
□ Yes
□ No
• Physician obtains results of necessary lab studies (Goal: within 45 minutes of being ordered).
□ If all criteria for t-PA administration are met, explain risks/benefits to patient and family. Risks include death; stroke; permanent neurologic injury; worsening of stroke symptoms
from swelling or bleeding in the brain; bleeding other parts of the body; need for blood transfusions to replace blood or clotting factors; other unexpected complications.
□ Obtain written informed consent, if possible.
□ Pharmacy is called to order t-PA (Pharmacy staff will need patient’s name, weight and medical record number).
□ Patient’s estimated/stated weight: __________ . Calculated dose for tPA: __________ mg. t-PA arrives in the Emergency Department.
□ If onset of stroke is still less than 3 hours, start tPA at 0.9mg/kg (but not exceeding 90mg) with 10% as bolus dose & the remainder given over the following hour.
□ t-PA administration is started (Goal: within 60 minutes of patient arrival).
□ Monitor for unexpected bleeding: (see Stroke Management Policy) Intracranial Hemorrhage Algorithm if patient develops signs/symptoms of bleeding.
□ Maintain blood pressure less than 180/110.
□ Patient receiving t-PA must not receive antithrombotic or antiplatelet agents for 24 hours (e.g., aspirin).
DISPOSITION
Admit to: □ ICU bed
□ Nursing Unit: ______________________
□ Home/Other: _____________________________
□ AMA
Comments: __________________________________________________________________________________
Physician’s Signature & Credentials: _______________________________________ Printed Name: __________________________ Date: ___________ Time: ___________
FORM #25861 (8/04)
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1 2
2








