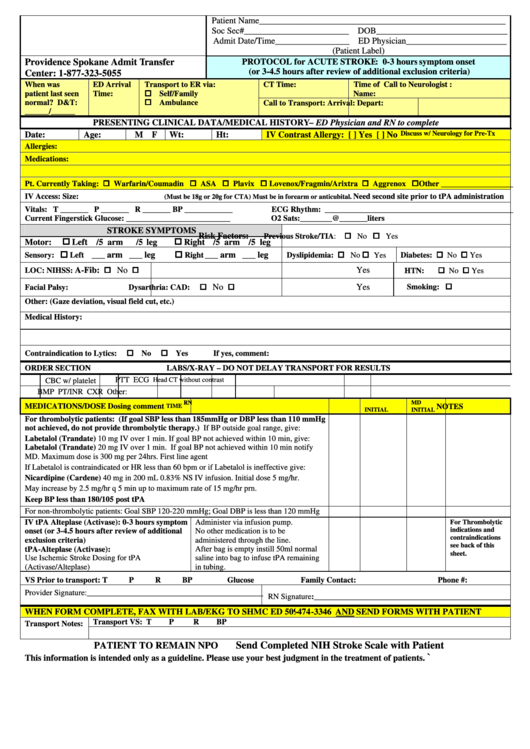
Clinical Data/medical History
ADVERTISEMENT
Patient Name_________________________________________________________
Soc Sec#________________________ DOB______________________________
Admit Date/Time_________________ ED Physician_______________________
(Patient Label)
PROTOCOL for ACUTE STROKE: 0-3 hours symptom onset
Providence Spokane Admit Transfer
(or 3-4.5 hours after review of additional exclusion criteria)
Center: 1-877-323-5055
When was
ED Arrival
Transport to ER via:
CT Time:
Time of Call to Neurologist :
Self/Family
patient last seen
Time:
Name:
Ambulance
normal? D&T:
Call to Transport:
Arrival:
Depart:
______/______
PRESENTING CLINICAL DATA/MEDICAL HISTORY – ED Physician and RN to complete
Date:
Age:
M F
Wt:
Ht:
IV Contrast Allergy: [ ] Yes [ ] No
Discuss w/ Neurology for Pre-Tx
Allergies:
Medications:
Pt. Currently Taking: Warfarin/Coumadin ASA Plavix Lovenox/Fragmin/Arixtra Aggrenox Other __________________
IV Access: Size:
Need second site prior to tPA administration
(Must be 18g or 20g for CTA) Must be in forearm or anticubital.
Vitals: T _______ P _______ R _______ BP ____________
ECG Rhythm: _______________________________________________
Current Fingerstick Glucose: __________________________
O2 Sats:________@_______liters
STROKE SYMPTOMS
Risk Factors:
Previous Stroke/TIA: No Yes
Left /5 arm
Right /5 arm /5 leg
Motor:
/5 leg
___ arm ___ leg
___ arm ___ leg
Dyslipidemia: No Yes
Diabetes: No Yes
Sensory:
Left
Right
A-Fib:
No
Yes
No Yes
HTN:
LOC:
NIHSS:
No
Yes
Smoking:
Facial Palsy:
Dysarthria:
CAD:
Other: (Gaze deviation, visual field cut, etc.)
Medical History:
No
Yes
Contraindication to Lytics:
If yes, comment:
ORDER SECTION
LABS/X-RAY – DO NOT DELAY TRANSPORT FOR RESULTS
CBC w/ platelet
PTT
ECG
Head CT without contrast
BMP
PT/INR
CXR
Other:
RN
MD
MEDICATIONS/DOSE
Dosing comment
NOTES
TIME
INITIAL
INITIAL
For thrombolytic patients: (If goal SBP less than 185mmHg or DBP less than 110 mmHg
not achieved, do not provide thrombolytic therapy.) If BP outside goal range, give:
Labetalol (Trandate) 10 mg IV over 1 min. If goal BP not achieved within 10 min, give:
Labetalol (Trandate) 20 mg IV over 1 min. If goal BP not achieved within 10 min notify
MD. Maximum dose is 300 mg per 24hrs. First line agent
If Labetalol is contraindicated or HR less than 60 bpm or if Labetalol is ineffective give:
Nicardipine (Cardene) 40 mg in 200 mL 0.83% NS IV infusion. Initial dose 5 mg/hr.
May increase by 2.5 mg/hr q 5 min up to maximum rate of 15 mg/hr prn.
Keep BP less than 180/105 post tPA
For non-thrombolytic patients: Goal SBP 120-220 mmHg; Goal DBP is less than 120 mmHg
Administer via infusion pump.
IV tPA Alteplase (Activase): 0-3 hours symptom
For Thrombolytic
indications and
No other medication is to be
onset (or 3-4.5 hours after review of additional
contraindications
administered through the line.
exclusion criteria)
see back of this
tPA-Alteplase (Activase):
After bag is empty instill 50ml normal
sheet.
Use Ischemic Stroke Dosing for tPA
saline into bag to infuse tPA remaining
(Activase/Alteplase)
in tubing.
VS Prior to transport: T
P
R
BP
Glucose
Family Contact:
Phone #:
Provider Signature:____________________________________________
RN Signature:_________________________________________________
WHEN FORM COMPLETE, FAX WITH LAB/EKG TO SHMC ED 509-474-3346 AND SEND FORMS WITH PATIENT
Transport VS: T
P
R
BP
Transport Notes:
Send Completed NIH Stroke Scale with Patient
PATIENT TO REMAIN NPO
`
This information is intended only as a guideline. Please use your best judgment in the treatment of patients.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1








