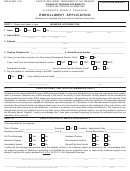
Enrollment Application Page 2
ADVERTISEMENT
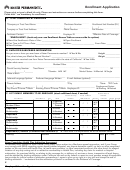
AUTOMATIC PAYMENT
(Not available for COBRA health plans)
CHECKING OR SAVINGS ACCOUNT
Savings
Note:
1. If your financial institution is a loan and savings bank, credit union or money
Type of account:
Checking
market fund, you must verify the specific requirements for an electronic transfer of funds
(ACH). 2. This application must be accompanied by your first payment. 3. This service
(electronic debit) will be effective on the month following the submittal of your
Routing Number (ABA)( 9 digits):
application.
Applicable Terms:
1.This authorization will remain in effect until a letter of cancellation
from the client is received, granting enough time for the insurer and the bank to make the
Account Number:
appropriate changes. Said notice can be submitted at our offices or service centers or it can
be mailed to Triple-S Salud, Attn, Departamento de Crédito y Cobro, PO Box 363628, San
Juan, PR 00936-3628 or faxed to (787) 774-4804 or (787) 749-4197. If the bank account
Name of Bank or Financial Institution:
changes in any way, it is the client’s responsibility to notify it at least 30 days in advance and
to fill out a new Automatic Payment form. 3. The bank account statements will be the
payment receipts. 4. Triple-S Salud reserves the right to end this form or payment and your
Name of bank account owner:
participation in it.
I authorize Triple-S Salud to originate electronic debits to my account located in the
specified bank or financial institution
Authorization Code:
Important Note:
If the bank account is not in the name of the plan member, then the
___ 09: Debit on the 19th of each month
___ 03: Debit on the 4th of each month
account holder must sign this authorization. If the debit day is a holiday, the debit will take
___ 99: Debit on the 27th of each month
place on the next business day.
___ 07: Debit on the 11th of each month
Law number 18 of January 8, 2004 establishes that:
Any person who knowingly and with the intention of committing fraud submits false information on an insurance application or who presents, orders or aids in the presenta-
tion of a fraudulent claim for the payment of a loss or other benefit, or presents more than one claim for the same damage or loss, will incur in a felony and, if convicted, will
be sanctioned for each violation with a fine no less than five thousand dollars ($5,000) and no greater than ten thousand dollars ($10,000) or a penalty of imprisonment for a
fixed term of three (3) years, or both penalties. In light of aggravating circumstances, the fixed penalty established could be increased to a maximum of five (5) years; if there
are extenuating circumstances, it can be lowered to a minimum of 2 (two) years.
PREMIUM PAYMENT
Both the Employer and the insured person will be jointly responsible for the payment of the policy’s premium, provided that said responsibility will cover all premiums due until
the policy’s date of termination, in accordance with the policy’s TERMINATION clause.
Triple-S Salud reserves the right to collect the premium due or, at its discretion, it may recover the costs incurred in the payment of claims for services rendered to the insured
person after the cancellation of said person’s health plan; provided that the insured person will be responsible for the payment of any of the two amounts claimed by Triple-S
Salud, except for the provisions contained in the policy’s Conversion Clause.
Triple-S Salud reserves the right to give a detailed report to any credit reporting agency, institution or organism on the default in payment by the employer or the insured person.
Being also provided that the debtor shall bear legal costs, expenses and fees, as well as any other additional expense Triple-S Salud incurs to collect the debt.
INSTRUCTIONS:
All shaded sections are the sole use of Triple-S Salud. Please be sure to read the Certificate of Benefits carefully.
1. Type or handprint in ink the information in the application. Fill out all the blocks in the application, except those that are shaded.
2. All names must be written as follows: last name, name and middle initial.
3. The basic coverage (hospital, medical-surgical and ambulatory), as well as the dental, pharmacy and major medical coverage will apply according to what is established in the
policy.
4. Optional dependents may choose similar or fewer services, but not more services than the main plan member. The Major Medical Coverage is not available for optional
dependents. Optional dependents over age 65 are not eligible for pharmacy coverage.
5. To be eligible to Triple-S Salud Care Plus Coverage, the person must have Medicare Parts A and B. The person must submit the documents to evidence Medicare Parts A and B
coverage and a copy of the Birth Certificate.
6. Hospital and Basic Medical Services offered in Esssencial Plans are only available for the employee; these plans do not cover optional dependents. Esssencial plans do not offer
pharmacy coverages, major medical expenses, Care Plus and services in the United States. The hospital plan does not offer ambulatory services, except emergency room services.
7. Please be sure that the information you provide is complete and accurate. Sign and date the application.
OBSERVATIONS:
COBRA ACT
By signing this application I commit to pay the premium required to ensure continuity of group benefits for me and my eligible dependents, if any, included in this application. I
also understand that the amount of this premium may vary at any moment there is a change of status or when the group policy is renewed. I understand that the benefits under
this coverage shall expire (1) once a period of 18 or 36 months has elapsed, as applicable; 2) if I do not pay the premium or ,(3) if my current eligibility status changes. Once the
plan is cancelled for lack of payment or for other valid reason I know that I will not be able to enroll in the coverage herein provided. Even more, I know that this coverage may
end if the coverage the employer offers to its active employees is cancelled. Enclosed with this application is the check or money order for the payment of the premium
corresponding to the period from the coverage effective date to the month of _______________________.
EMPLOYER CERTIFICATION (COBRA)
I hereby certify that the person that subscribes this application is eligible to continue receiving the benefits of the group plan under the provisions of COBRA for a maximum of
______ months. The premium to be paid in order to receive these benefits is _____, subject to verification by the insurance company. We authorize said company to keep the
applicant under our group coverage. We understand it is our duty, as employer, to deal the billing and collection process directly with the beneficiary and to pay the insurance the
premium amount owed so the person can continue coverage under COBRA. Included is the corresponding premium payment, as previously calculated.
I HEREBY CERTIFY
that the information in this application is accurate and true; that I have never, directly or indirectly, presented a fraudulent claim or any false
evidence to support a claim with the purpose of obtaining a payment according to the insurance contract; and, I authorize Triple-S Salud to verify these facts and this information
and to cancel my health insurance plan if what I hereby certify is not true.
In case the policy is cancelled, I will assume the responsibility of the health service costs rendered to any plan member insured under this policy, as of the cancellation date; and
that by assuming this responsibility I do not limit Triple-S Salud’s right to take any legal action against me as long as this legal action is initiated in conformance with the Law
GROUP NAME
SIGNATURE OF GROUP ADMINISTRATOR
GROUP NUMBER
SIGNATURE OF APPLICANT
NAME OF APPLICANT
DATE (MONTH / DAY / YEAR)
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1 2
2